The Reading Room
Hospice care has so much to offer patients, families, and providers. But it can also be a bit confusing at times. That’s why we created The Reading Room. It’s a special place where people can learn and grow in their understanding of hospice any time of day. It’s like a whole library in the palm of your hand or with a click of your mouse. Welcome to The Reading Room!
We gratefully acknowledge the generous support of Elea Institute in helping fund The Reading Room.
Hospice and Palliative Care 101
Comparing Palliative Care and Hospice
What is the focus?
Palliative Care: The focus is on pain, symptoms and stress related to having a serious illness. Hospice Care: The focus is providing comfort through pain and symptom management, as well as spiritual and emotional support when curative treatments are no longer an option.
Who can receive this care?
Palliative Care: Anyone with a serious illness, regardless of life expectancy or prognosis. Hospice Care: Anyone with a serious illness that has a life expectancy of 6 months or less.
Can I continue to receive curative treatments?
Palliative Care: Yes, anyone receiving palliative care can pursue curative treatments. Hospice Care: Patients in hospice no longer receive curative treatments, however, they may continue to receive treatments that maintain quality of life and/or are comfort focused.
What services are provided?
Palliative Care: Pain and symptom management, in-person, and telephone visits. May assist with advance care planning and community referrals. Hospice Care: Pain and symptom management, in-person visits by different healthcare providers, medical equipment, volunteer services, spiritual care, bereavement, and counseling services.
Where are services provided?
Palliative Care: Palliative care may be provided in any setting like a private home, nursing home, assisted living facility. Hospice Care: Hospice care may be provided in any setting like private home, nursing home, assisted living facility.
Who provides these services?
Palliative Care: Most palliative services are provided by a Nurse Practitioner. Hospice Care: Hospice care is provided by physicians, nurses, social workers, chaplains, volunteers, nurses' aides, and other disciplines.
As the end of life draws near, the body is no longer able to digest and process food or fluids. This change happens gradually and is a normal and natural part of the dying process.
- Take your cues from your loved one when it is time to stop. As body functions slow down, your loved one may no longer feel hunger like they used to. The brain is signaled that food and fluids are no longer needed.
- As your loved one nears the end of life, it is common to lose the ability to swallow. This is also a sign that the body is no longer able to process food and fluids. Feeding someone unable to process the food may cause nausea, vomiting, or choking, as it cannot be digested.
- Instead of offering food or drink, this is the time to offer comfort in ways such as: gentle touch, conversation, prayers, music, or massage.
- It is okay to offer sips of water if your loved one is awake and alert enough to drink and swallow. Cool water can also be offered with an oral swab, which can provide enjoyment and comfort.
- It is common for people to breathe through their mouths at the end of life, which can lead to having a very dry mouth and lips. Using an oral swab with cool water to clean the mouth and lips is helpful and comforting. Use nonpetroleum based lip balm or moisturizer for the lips.
Can patients still receive medical treatment while on hospice?
- Hospice focuses on providing comfort care rather than curative treatments, however, patients may continue to receive treatments that help manage their symptoms and improve their quality of life. Talk with your hospice team regarding treatments and goals of care.
How long can a patient receive hospice care?
- Hospice care is provided if the patient meets the eligibility criteria and continues to have a prognosis of 6 months or less. Patients can choose to stop hospice care at any time if their condition improves or if they decide to pursue curative treatments.
Does choosing hospice mean giving up hope?
- Hospice does NOT mean a person is giving up hope! Hospice shifts the focus from curing an illness to focusing on quality of life and comfort. Patients and families can still hold onto hope by having meaningful experiences and by spending valuable time with their loved ones.
What happens if a patient’s condition improves while on hospice?
- If a patient’s condition improves to the point where they no longer meet the conditions for hospice care, they may be discharged from hospice. In a situation such as this, they can resume curative treatments or transition to palliative care, if indicated.
Can a patient keep their regular doctor while on hospice?
- Yes, patients can keep their primary physician while on hospice. The hospice physician will work together with the patient’s primary care physician to manage symptoms and coordinate treatment.
Is hospice only for patients with cancer?
- No, hospice is available to anyone with a terminal (life-limiting) illness. Some of the most common diagnoses in hospice are heart disease, Alzheimer’s disease, chronic obstructive pulmonary disease (COPD), end-stage kidney disease, liver disease, and stroke.
Myth: Hospice means giving up hope.
Truth: Hospice can help redefine hope. Hospice helps people maintain their dignity and quality of life by providing comfort-focused, individualized care.
Myth: Hospice is a place.
Truth: Hospice provides care to patients in their homes, or wherever a patient calls home such as an assisted living facility, a nursing home, or even in the hospital.
Myth: Everyone receiving hospice is given Morphine.
Truth: Morphine is a medication used by hospice to help manage distressing symptoms such as pain or shortness of breath. Not everyone needs Morphine, therefore, not everyone uses it. It is also important to know that all patients have a choice when it comes to medications being prescribed.
Myth: Morphine brings on death sooner.
Truth: Morphine is a very safe and effective medication when used properly. It does NOT hasten death, and it can help the patient have a better quality of life by relieving distressing symptoms.
Myth: Hospice is expensive.
Truth: Hospice is a benefit covered by Medicare, Medicaid, and most private insurance companies. Even if a person does not have insurance, many hospices have charitable foundations that can offer help during these situations.
Myth: Hospice should be considered only when the patient is close to death.
Truth: Hospice offers so many benefits both to the patient and the family that it is best to call hospice early on when medical treatments can no longer cure the patient’s disease. Hospice professionals can offer help with controlling pain, reducing anxiety, assisting with personal care, and bathing. Hospice can offer spiritual and emotional support as well.
Myth: People are not able to keep their family physician when they are with hospice.
Truth: The patient’s personal or family physician can stay on as part of the hospice care team. The hospice physician will work with the patient’s family physician to manage their care in the best way possible.
Myth: Eating and drinking are discouraged while receiving hospice care.
Truth: While receiving hospice care, patients are encouraged to eat and drink for pleasure. This means they should be offered food and drinks they will enjoy and can eat safely. During the dying process, there will come a time when the patient has little to no appetite and naturally stops eating and drinking. This happens when the body is no longer able to process food and fluids, and this is a very natural and expected part of the dying process.
Myth: Using a feeding tube during the dying process allows patients to live longer.
Truth: While each person’s situation is unique, artificial nutrition and hydration through a nasogastric tube (NG-tube), or a gastrostomy tube (G-tube) do not usually make the patient feel better or live any longer. This type of nutrition also comes with many complications, such as infections, vomiting, diarrhea, and aspiration.
Anyone can refer a person to be evaluated for hospice services including physicians, family members, or even the patient themselves. If you or someone you love needs hospice care and support, hospice is just a phone call away.
What information should be included with a referral?
- The person’s name, address, date of birth, and phone number.
- The referring person’s name, address, and phone number which includes the relationship this person has with the potential patient (i.e., primary physician, specialist, friend/relative, spouse, child, etc.)
- Primary caregiver’s name, address, and phone number.
- Diagnosis or brief history of disease.
Other information that is helpful to include:
- Current medication list.
- Recent labs or test results.
- Recent medical history and physical.
- Any current advanced directives (i.e. POLST, POA).
- Copy of Medicare or insurance card.
- Any recent progress notes from physician visits or
Talking about what matters to you and your wishes for care through end-of-life is important. Here are some helpful tips for having these difficult conversations.
- Think about what really matters to you. This can be started by thinking about what a good day looks like to you as well as who or what you feel supported by during difficult times.
- Plan your talk. Think about how you feel about certain situations that may arise now, in the future, and toward the end-of-life.
- Start talking. Have conversations with the most important people in your life regarding what matters most to you. Make your thoughts and feelings as clear as possible to others.
- Keep talking. Now that you have started the conversation, keep it going! The more you keep talking to others, the more likely it is your wishes will be known and remembered by those who are close to you.
- The following is a list of “What Matters Most” ideas to think and talk about with your loved ones. Choose which is most important and continue through to the least important.
| To be pain-free | To not have anxiety | To be able to breathe easy |
| To be kept clean | To have human touch | To have my financial house in order |
| To prepare my family for my death | To die where I want to | To know the changes my body will go through |
| To know that I lived my life well | To say goodbye to those who matter most to me | To be able to recall personal accomplishments |
| To take care of unfinished business | To prevent arguments later by talking with my family now | To have an advocate who speaks well on my behalf |
| To be treated the way I want to be treated | To keep my dignity | To keep my sense of humor |
| To have a doctor who really listens to me | To have my friends close by | To not die alone |
| To have someone who really listens to me | To have a doctor I can trust | To have a nurse who makes me feel comfortable |
| To be mentally aware | To have my funeral all planned out | To not be a burden to my family |
| To be able to help others | To be at peace with God | To be able to pray |
| To be free from life-supporting machines | To be able to talk about what frightens me |
There are four levels of hospice care, as defined by The Centers for Medicare and Medicaid. Each level of care is designed to meet your loved one’s unique needs throughout their hospice journey. The four levels of care are:
1) Routine Hospice Care – This is the most common level of care. Patients typically receive care in their own home, or wherever they are currently living. This may be in an assisted living facility, a nursing home, or even in another family member’s home.
2) Continuous Care – This is care that is provided by the hospice nursing team for up to 24 hours per day for a brief period. This is done to support the person and the caregiver during a time of crisis, such as when your loved one is experiencing severe symptoms like pain. The goal of continuous care is to get symptoms under control while keeping your loved one out of the hospital. Situations that may be appropriate for continuous care:
- Uncontrolled Pain.
- Difficulty Breathing.
- Uncontrolled Agitation.
- Seizures.
3) Inpatient Care – This level of care is provided in a hospital setting. This level of care is appropriate when your loved one experiences severe symptoms that cannot be controlled or managed at home. Your loved one will remain in hospice care while in the hospital, with the goal of getting symptoms under control and getting your loved one home as quickly as possible.
4) Respite Care – This level of care is focused on giving caregivers the ability to have time away from the pressures and stress of caregiving. Respite care provides a temporary break for the caregiver by having your loved one go to a nursing home for care. The stay is to be no more than 5 consecutive days with your loved one still receiving hospice services.
Talking about dying with a loved one can be incredibly challenging but also deeply meaningful. Here are a few suggestions for having these difficult conversations.
- Choose a quiet, comfortable space where you won’t be interrupted.
- Start the conversation by expressing care and concern for your loved one. Let them know you are there to support them.
- Let your loved one guide the conversation. Respect their pace and comfort level when discussing dying.
- Be mindful of your words and tone. Use gentle, empathetic words to express love, support and understanding.
- Create a safe space for your loved one to share their feelings, fears, and wishes regarding their illness and end-of-life care. Listen actively and without judgement.
- Use open-ended questions to encourage your loved one to express themselves. For example, “What are your biggest concerns or worries?”
- Offer reassurance and comfort. Let your loved one know their feelings are valid.
- Respect your loved one’s choices regarding end-of-life care.
- When the time is right, discuss practical matters such as advanced directives, funeral arrangements, and financial planning. This can also provide peace of mind for everyone involved.
- Continue the conversation and check in with your loved one regularly. Let them know you are there for them whenever they need to talk.
Most people are not prepared for the overwhelming feelings that can be experienced after the loss of a loved one. Grief is the natural emotional response to the loss of someone close. It is experienced differently by each person and is shaped by your relationships, by the changes related to the loss of a loved one, by your previous experiences, and by your surrounding support system.
- Grief is a normal and natural response to loss.
- There is no “right” way to grieve.
- There is no timeline for grief to “be over”.
- Grief can produce physical and emotional responses such as anxiety, headaches, anger, shock, and sadness.
Mourning is an expression of grief that follows a loved one’s death. It is expressed as crying, talking about the death of the loved one, sharing stories, and many other actions. Mourning after the death of a loved one is necessary because it helps you begin to heal. Everyone mourns differently, but most people go through similar experiences such as:
- Accepting the reality of the loved one’s death.
- Embracing the pain of loss.
- Remembering the person who died.
- Developing a new self-identity.
- Searching for meaning.
- Receiving support from others.
Bereavement is the experience of losing someone important to us. It usually involves feelings of grief and sadness, but it’s possible to experience a wide range of emotions. Each person’s experience is unique, and it’s important to know that there’s no right or wrong way to feel.
- Bereavement care is a service provided by a hospice providing support to help you deal with grief after the loss of a loved one.
- As part of the Medicare hospice benefit, family and caregivers of the hospice patient have access to bereavement care for 13 months following the death of their loved one.
- Bereavement services provided by hospice range from support groups, memorial services, informational and educational resources, grief counseling, and referrals to appropriate community resources.
- Hospice bereavement programs facilitate healthy grieving and aim to prevent grief-related health issues and/or mental health problems.
- Hospice offers a unique blend of services including medical, emotional and spiritual care that focuses on relieving suffering and symptoms for patients as they near the end of life.
- Hospice focuses on improving quality of life and honoring the wishes of the patient and family.
- Hospice gives each patient the opportunity to live their final months more fully and on their own terms in their home or wherever they currently call home.
- Hospice provides a specially trained team of people who work together to address each patient’s medical, emotional and spiritual needs. This team includes a physician, nurse, hospice aide, social worker, chaplain, volunteer, and bereavement specialist.
- Hospice care is for anyone who:
- is in the terminal phase of any life-limiting disease or illness defined by Medicare as a life expectancy of 6 months or less.
- is seeking comfort-focused care, not curative treatments.
If you are unsure if you or your loved one is appropriate for hospice, please reach out to your physician or give Northern Illinois Hospice a call.
- Palliative care is a specialized type of care focused on easing pain and discomfort, reducing stress, and helping people who have a serious disease or illness to have quality of life.
- Palliative care is appropriate for anyone who has a serious disease or illness and struggles to manage symptoms and/or has been to the Emergency Department or hospitalized frequently related to the illness.
- Palliative care is provided in coordination with a patient’s current physician and can be done while seeking curative treatments such as chemotherapy, radiation, dialysis, and surgery.
- Palliative care can be provided at any stage of a disease and does NOT require the patient to have a life expectancy of 6 months or less, such as with hospice care.
- Palliative care can be provided in any setting, such as the patient’s home, hospital, nursing home, or assisted living facility.
If you are unsure if you or your loved one is appropriate for Palliative Care, please reach out to your physician or give Northern Illinois Hospice a call.
Once your loved one and your family agree hospice is the best choice, then admissions orders are received, and paperwork is signed. Your loved one is now officially admitted to hospice care. The first visit, also known as the “admission visit” may be longer than other visits as essential information is gathered. An initial assessment of your loved one will be completed along with ordering of equipment, supplies, and medications, as appropriate. After the admission visit, you will be contacted by many different members of the hospice team. Individual team members will work with you to schedule convenient visits. Some visits may be daily, while other visits may be weekly, monthly, or more frequently depending on the needs of you and your loved one. Visits may also be requested whenever needed. The hospice team consists of:
- RN Case Manager
- Chaplain
- Social Worker
- Certified Nursing Assistant (CNA)
- Volunteers
- Hospice Physician/Hospice Nurse Practitioner
- Complementary Therapists i.e., Music, Massage, Pet, and Aromatherapy
- Additional Nursing support i.e., LPNs and RNs
- Bereavement coordinators
Medical equipment, supplies; and medications related to symptom management, the primary illness and related medical conditions will be delivered usually within the first 24-48 hours after the initial admission visit. The hospice team will provide physical, emotional, and spiritual support to your loved one and your family during visits. This includes bit is not limited to monitoring pain, managing symptoms, addressing emotional issues, addressing spiritual issues, and offering support and resources as needed. The hospice team will also provide instruction to your primary caregiver on how to provide the best care possible for your loved one.
Advanced Care Planning and Resources
Advanced Directives and Special Considerations Based on Diagnosis
There are certain diseases that require special thought and attention when it comes to creating advanced directives.
Alzheimer’s Disease/Dementia – Alzheimer’s is a progressive disease, which means it gets worse with time. If someone with Alzheimer’s lives long enough, they will most likely get to a point where they are unable to communicate their wishes. This is why having advanced directives in place early is so important.
Cancer – Goals of care often change throughout the cancer treatment journey, especially if cancer becomes chronic or terminal. If this happens, it is important to consider what treatments – such as chemotherapy, radiation, and blood transfusions – will be continued and if the benefits and risks are in alignment and support the goals of care. Chronic Obstructive Pulmonary Disease (COPD) – This disease often has periods of “flare-ups” when symptoms are difficult to manage, along with short periods of improvement, but eventually it can become terminal or life-ending. Goals of care often change throughout the COPD journey. It is important to consider what treatments – such as antibiotics and mechanical assistance with breathing – will align with the goals of care as the illness progresses.
Kidney Failure – As kidney failure progresses, dialysis becomes the only option to stay alive. Even with the best care and support, eventually the physical and emotional toll of dialysis sometimes outweighs the benefits. It is important to consider what the goals of care are and if dialysis continues to be in alignment with these goals as the illness progresses.
What is Financial Caregiving
Financial caregiving is a term used to describe managing the personal finances of a seriously ill or elderly person who requires assistance – including paying bills, overseeing bank accounts, filing taxes, and taking on financial power of attorney.
How to Provide Financial Caregiving
- Talk about finances with the person you are caring for. Try to get a picture of their financial situation, including areas of concern. This can be difficult, but it’s an important step to understanding their financial situation.
- Be sensitive to the person’s need for independence. Consult with the person you are helping. Offer to start with small tasks, such as paying bills or balancing the checkbook.
- Get input from other people, if appropriate. If there are others that want to help or be involved, include them sooner than later - if the person you are caring for agrees.
- Make a list of all expenses and debts. This includes utilities, mortgage or rent, car payments, insurance, real estate taxes, and more.
- Document all income. This includes social security, pensions, retirement distributions, survivors’ benefits, and more.
- Create a budget. A budget should include all income and expenses, including both fixed and irregular ones. Plan for how to pay for all expenses, and plan for cost of living to increase with time.
- Make an inventory of accounts. This should include all accounts, insurance policies, credit cards, website user IDs and passwords. Keep this information private, safe and secure.
- Get access to accounts. This can be as simple as getting your name added to accounts as a joint account holder or having the primary account holder give verbal agreement authorizing you to speak on their behalf.
- Get authorization to speak on behalf of care recipient. This can be made official by executing a durable power of attorney for finances.
- Simplify and automate. Set up auto-pay for all regular bills. Only keep open the credit card accounts that are necessary. Consolidate assets, if appropriate.
- Limit risk and keep records. If the person you are caring for has cognitive issues, it may help to have a credit card with a low limit or a debit card from a bank account with a small balance – just to be safe.
- Don’t forget about taxes. Income taxes will still need to be filed, real estate taxes need to be paid, and required minimum distributions (RMDs) from retirement accounts still need to be made.
Long-Term Care Options
There are different options available for long-term care – depending on your needs and financial situation.
- Assisted Living Facility (ALF): This type of facility provides seniors with non-medical care and supervision. This level of care is appropriate for people who need assistance with daily activities but are still able to maintain some independence. The staff can offer help with medication management, personal care, housekeeping, laundry, meals, and social activities. This is paid for by the individual and is not covered by Medicare or Medicaid. This may be partially paid for by long-term care insurance.
- Supportive Living Facility (SLF): This type of facility provides seniors with the same or similar care as an assisted living facility; however, this type of facility accepts Medicaid for payment.
- Skilled Nursing Facility (SNF): The type of facility provides temporary care for people with more advanced nursing or health care needs. This may also be referred to as “rehab” after a hospital stay, because it offers nursing and therapy services. Medicare and/or Medicaid may pay for this for a brief time, but there are specific conditions that must be met.
- Nursing Home or Long-Term Care Facility (LTC): This type of facility may offer long-term 24/7 care that includes some medical assistance. This type of care may be offered in the same building as the SNF. Some nursing homes accept Medicaid, but there are conditions for this to apply. Medicare may pay for some of the skilled nursing services, but not for the non-skilled care. This type of care may also be paid for privately or with long-term care insurance.
- Home Health Care: This is a type of care provided to patients in their home. This may be covered by Medicare, Medicaid, or private insurance if you are homebound and need short-term, intermittent skilled nursing or therapy services. This type of care requires a doctor’s order.
- Caregiving Services: This is a type of care provided to patients in their home usually for longer periods of time each day. Services provided are typically assistance with personal care, housekeeping, cooking, and companionship. Caregiving services may be paid for by Medicaid, the VA (for veterans only), long-term care insurance, or private pay. If you have Medicaid, a family member can qualify to be a paid caregiver through the Illinois Department on Aging and the Community Care Program. For more information, please visit https://ilaging.illinois.gov/programs/ccp.html.
- Hospice: This is a type of care provided when you have a terminal, or life-limiting condition. It is provided wherever you call home, and is covered by Medicare and Medicaid, as well as by most private insurance companies.
Medicaid Spenddown Program
What is the Spenddown Program?
• The spenddown program helps some people who have too much income or too many assets like bank accounts and other resources to qualify for Medicaid and possibly other medical programs. If you have medical bills or receipts for recent payments made for medical care, you may qualify under spenddown to get a medical card to pay for some of these expenses.
• Spenddown works a little like an insurance deductible. You pay for the cost of your medical care up to a set amount each month based on your income and assets. This is called your spenddown amount.
• Once you can show bills or receipts for medical care, drugs or supplies that are equal to your monthly spenddown amount, you can get a medical card to pay for other medical care you need for a month.
• Pay-in spenddown lets people pay the spenddown amount each month instead of submitting bills. This is like paying a health insurance premium each month. Not everyone can have pay-in spenddown.
Medicare and Medicaid
Medicare is federal health insurance for anyone age 65 and older, and some people under 65 with certain disabilities or conditions.
Medicaid provides health coverage to millions of Americans, including eligible low-income adults, children, pregnant women, elderly adults and people with disabilities. The program is funded jointly by the state and the federal government.
- If you qualify, you can have both Medicare and Medicaid.
- People who have both Medicare and full Medicaid coverage are “dually eligible.” Medicare usually pays first when you are dually eligible, and you receive Medicare-covered services. Medicaid usually pays last, after Medicare and any other health insurance you have.
- If you are dually eligible, Medicare covers your prescription drugs. You will automatically be enrolled in a Medicare drug plan that will cover your drug costs instead of Medicaid. Medicaid may still cover some drugs that Medicare doesn’t cover.
- You might be able to still get Medicaid if you meet your state’s resource limit, but your income is determined to be too high to qualify. Some states will let you “spend down” the amount of your income that is above the state’s Medicaid limit. You do this by paying non-covered medical expenses and cost sharing like Medicare premiums and deductibles until your income is lowered to a level that qualifies you for Medicaid.
Virtual and Online Support Groups and Resources
Compassionate Friends: This organization provides support for the loss of a child of any age which includes resources, listings of events and groups. https://www.compassionatefriends.org/
Dougy Center for Grieving Children and Families: The Center provides support which Includes guidance, tip sheets, activities, podcasts, and a variety of toolkits. https://www.dougy.org/
Grief in Common: This forum allows those grieving to create a profile that outlines who you are, who you have lost and the circumstances surrounding that loss. The hope is for the griever to find a connection with someone who understands. https://www.griefincommon.com/
Grieving.com: This is a community of people supporting each other through the loss of a partner, child, other family member or friend. https://forums.grieving.com/
National Alliance for Children’s Grief (NACG): This organization provides information and support for children and teens grieving a death which includes education and resources. https://nacg.org/
Thanacare: This online resource includes free, 45-minute sessions with advocates available to speak with individuals about the care they wish to receive and provides access to professional support and guidance in the advanced care planning process. https://www.thanacare.com/
The Conversation Project: This guide discusses how to talk with a child living with a serious illness about the health care that is right for them. https://theconversationproject.org/wp-content/uploads/2020/12/PediatricGuide.pdf
The Dinner Party: This is an online community of 21–45-year-olds who have experienced the loss of a parent, partner, child, sibling, other close family member or friend. https://www.thedinnerparty.org/
What is an Advanced Directive?
An advanced directive is a written record that gives your doctor or other healthcare provider(s) information about your personal wishes and what is important to you in the event you are sick and unable to speak for yourself.
Two types of Advanced Directives in Illinois
- Healthcare Power of Attorney: This is a document that defines who the person is that will speak on your behalf regarding your healthcare when you are unable to do so. This is important because if you are too sick or injured to speak for yourself, you need someone you trust to represent you and your wishes.
- Living Will: This is a document that defines what your wishes are regarding medical treatments, what you do and do not want, in the event you cannot speak for yourself. Completing the “Five Wishes” book may be helpful in communicating your healthcare wants and goals.
For more information, please visit https://www.caringinfo.org/wp-content/uploads/Illinois.pdf or https://www.fivewishes.org/ or https://dph.illinois.gov/topics-services/health-care-regulation/nursing-homes/advance-directives.html
What is the POLST Form?
The Practitioner Order for Life-Sustaining Treatment form (POLST) expresses your choices regarding medical decisions if you are unable to speak for yourself. The POLST is different from a living will because it is signed by a doctor and becomes a medical order. While the POLST form is voluntary, the form is important to have if you are seriously ill. The POLST form allows you communicate your wishes with someone you trust and with the health care professionals involved in your care by addressing several critical decisions that may occur at the end of life. The POLST has options regarding:
- Do Not Attempt Resuscitation (DNAR/DNR): This choice states you do NOT want CPR (cardiopulmonary resuscitation) attempted if your heart stops beating.
- Intubation/Ventilation: This choice states whether you want a machine to assist or to do the work of breathing for you, if you are not breathing on your own.
- Medications/IV Fluids – This choice states whether you want certain medications, or IV fluids used to prolong your life.
- Artificial Nutrition: This choice states whether you want nutrition given to you through a tube or IV. This is also known as having a “feeding tube.”
- Comfort-Focused Treatments: This is what people in hospice typically elect, as it focuses on treatments that provide comfort. Care is focused on the primary goal of relief from pain or suffering by using medications or other treatments like oxygen. The focus is to maximize comfort and quality of life.
For more information on the State of Illinois POLST form, please visit: https://www.polstil.org/information-for-individuals-caregivers/
When is a Caregiver Needed?
When people are sick or as they grow older, they may face new challenges with caring for themselves due to physical or mental changes. A decline in their ability to care for themselves does not always necessitate a move to assisted living or to a nursing home, but it does indicate a need for extra help to support a person’s desire to age in place safely. The following are some signs that it may be time to hire a caregiver for your loved one:
- Change or stopping regular activities;
- Poor personal grooming;
- Not taking medications;
- Memory issue/forgetfulness;
- A messy house;
- Bruising/new injuries/falls;
- Not dressing appropriately;
- Difficulty driving;
- Inability to keep up with or pay bills; and/or
- Holding onto furniture and walls to get around the house.
Basic caregiver duties may include:
- Assisting with bathing, grooming, and dressing;
- Doing laundry;
- Preparing meals and shopping for food;
- Doing light housekeeping;
- Managing and monitoring medications;
- Assisting with transportation;
- Assisting with walking and mobility;
- Providing companionship and emotional support; and/or
- Communicating with doctors.
Safety at Home and How Tos
Preventing Falls in the Home
Falling at home can lead to serious injuries – such as cuts, bruises, and even broken bones. To help keep you and your loved one safe, here are some simple steps you can take to help prevent falls.
- Use your assistive device! (walker, cane, etc.)
- Remove any throw rugs.
- Arrange furniture so there is a clear path for walking.
- Wear supportive shoes.
- Avoid wearing just socks or loose slippers.
- Be aware of any side effects from medications such as dizziness, so change position slowly.
- Always keep a phone nearby.
- Improve lighting in the home, for example brighter light bulbs, nightlights, etc.
- Use a “reacher grabber” tool to pick up items from the floor or items out of hand’s reach.
- Add grab bars in your shower and/or tub.
- Use a rubber non-slip mat in your shower and/or tub.
- Clear any wires and cords from walkways.
- Get dressed while sitting down.
- Get up slowly from lying down or sitting and stay sitting if you are feeling dizzy and/or lightheaded.
Mobility and Safe Transfers
Learning how to move and get around your home safely is important, so you do not get hurt. Here are some tips to help keep you safe.
- Change positions slowly especially when getting up from a sitting or lying down position.
- Use small steps to approach the surface to sit on e.g., bed, chair, toilet, etc.
- Reach back to feel the chair seat or armrests with both hands; do not sit unless the surface is located with your hands and you can feel the chair on the back of your legs.
- When rising out of a chair, push up from the chair with both hands; come to a standing position making sure you are steady and have your balance; then put both hands on your walker or cane.
- Know how to use your assistive device safely e.g., cane, walker, wheelchair, etc. If you do not know how to safely use your devices, ask your hospice nurse to show you.
- Ask your hospice nurse about devices that might help you function more safely, such as a walker, a lift, or a bedside commode (portable toilet).
Safety with Eating and Drinking at End of Life
It is normal for a person nearing the end of life to lose their appetite or their desire for food and drink. Here are some important food and drink safety considerations.
- To prevent choking, offer food and fluids only when your loved one is awake, alert, and able to sit up.
- Offer foods of similar consistency as foods with a variety of textures may cause choking. Offer easy to chew foods, if they want to eat.
- When your loved one nears the end of life, giving nutrition or fluids through an IV or a feeding tube may cause discomfort and/or other problems.
- If your loved one is awake, offering ice chips may provide comfort and enjoyment.
- Offer a sippy cup or use a straw if weakness makes it difficult for your loved one to hold a cup.
- Offering food and fluids is fine, but do not pressure or force. Not eating at the end of life is normal and forcing your loved one to eat or drink may cause pain.
- Eating when your loved one is not hungry or unable to eat safely can cause nausea, vomiting and/or choking. If nausea is an issue, serving very small portions of easy-to-swallow foods and liquids may help.
- Provide mouth care at least twice a day, even if your loved one is no longer eating or drinking. If your loved one is sleeping with their mouth open, you can provide oral care as often as every 1-2 hours.
Preventing Infections
Infections occur when germs are spread from one person to another. This commonly happens because of unclean hands, so having clean hands is the best way to prevent infection! Here are some tips on how to prevent infections.
- Wash your hands often, especially before and after providing care for your loved one.
- Use soap and warm water to wash your hands for at least 20 seconds. Singing “Happy Birthday to you” twice through is approximately equal to 20 seconds.
- Rinse hands well and dry with a clean towel or a paper towel.
- Hand sanitizer rubs or sprays may be used if your hands are not visibly soiled.
- Ask visitors to wash their hands before visiting.
- Avoid others who are sick and use a mask if needed.
- Clean and disinfect surfaces in home regularly especially those frequently touched by others.
Skin Care
Skin care is an essential part of providing care for your loved one. Protecting skin from injury or breakdown is important, especially if your loved one is staying in the same position for much of the day and/or has issues with incontinence. Here are some tips for maintaining healthy skin.
- Wash skin with warm water and mild soap.
- Avoid friction or rubbing.
- Cleanse skin after soiling.
- After cleansing, apply moisture barrier creams to areas of skin that are likely to be in contact with moisture such as the buttocks.
- Keep your loved one’s heels off the bed by putting a pillow underneath their calves and knees for support. Your hospice nurse or aide can show you how to position.
- Change your loved one’s position every 2 hours while they are in bed.
- Use pillows to protect your loved one's bony areas, such as heels, elbows, and knees from lengthy periods of pressure to prevent bed sores.
- Keep the head of the bed at a 30-degree angle or less when your loved one is not eating or drinking if comfortable for them.
How To Use an Oxygen Tank
Oxygen therapy can be used to treat symptoms such as shortness of breath and may provide comfort at the end of life. When oxygen is used, it is important to know how to use it safely. Here are some tips for safe oxygen use.
How to Turn On an Oxygen Tank
- Make sure the oxygen tank is secured in an upright stand.
- Use the cylinder wrench or toggle to turn the oxygen cylinder valve by at least a half turn counterclockwise.
- Check the pressure gauge to verify there is enough oxygen in the tank, usually 2,000 psi.
- Adjust liter flow using the dial on the regulator to the correct oxygen flow.
How to Use Oxygen
- Attach tubing with nasal cannula to the oxygen regulator nipple.
- Place the two prongs of the nasal cannula in your loved one’s nostrils. The end of the curved part of the prongs should point downward.
- Loop the tubing over the ears and adjust the tubing so it is comfortable under the chin.
- Use the slider to tighten the tubing, if needed.
- Make sure your loved one is comfortable, and the oxygen is flowing at the correct flow rate by looking at the dial.
How to Turn Off an Oxygen Tank
- Use the cylinder wrench or toggle to turn the cylinder valve clockwise until completely off and closed.
Oxygen Safety Tips
- Keep all oxygen equipment at least 15 feet away from any type of open flame.
- Do not use petroleum-based ointments or lotions in or around your loved one’s nose or lips such as Vaseline or Vicks.
- Do NOT smoke or allow anyone else to smoke while oxygen is in use!
- Post OXYGEN IN USE/NO SMOKING signs wherever oxygen is being used.
- Store canisters in a secure and upright position.
- Store canisters in a well-ventilated cool area away from any heat sources and away from direct sunlight.
Who To Call in an Emergency
Your hospice care team is here to help you in any situation. Call the hospice anytime 24 hours a day/7 days per week. Your hospice team will help you determine what care is needed and what to do next. Call hospice first in the following situations:
- Your loved one falls.
- Any medical equipment failure, service issues, or loss of power.
- Any medication refill needs or questions.
- Any equipment or supply needs such as additional oxygen tanks or depends.
- Any sudden change in your loved one’s condition such as an increase in sleep, no longer responding, a change in eating habits, any new or continued agitation, change or increase in pain, etc.
Call 911 for the following emergency situations:
- To access emergency services such as the police department or fire department.
You always have the right to call 911, but most situations can be managed by your hospice team. If it is necessary to call 911 or go to the hospital, please notify the hospice first, so a team member can contact you or meet with you to discuss treatment options.
What to Do After Your Loved One Dies at Home
The death of a loved one is an emotional experience for the families and caregivers of the person who died. When a loved one dies at home, it is normal to feel overwhelmed and unsure about what to do and who to call. Hospice is here to help and guide you through this experience – every step of the way. Call the hospice first and a hospice nurse will then come to your home to help you. Once the hospice nurse arrives at your home, they will assist with:
- Officially confirming the death of your loved one.
- Washing and preparing your loved one’s body for transportation to the funeral home.
- Calling the funeral home to arrange transportation of your loved one’s body.
- Notifying the county coroner of your loved one’s death.
- Coordinating for the medical equipment to be picked up e.g., hospital bed, mechanical lift, oxygen, etc..
- Notifying the family physician of your loved one’s death.
- Calling any family as requested.
- Providing guidance regarding medication disposal and getting rid of any medical supplies e.g. depends.
- Providing comfort and support to you and your family as needed.
- Contacting additional resources for emotional support for you and your family such as a social worker, chaplain, or bereavement coordinator as needed.
How to Talk to a Loved One Who Is Dying
Saying goodbye to a loved one can be very emotional and difficult, but it is an important part of the grieving process, and possibly an important part of “letting go” for your loved one. Here are some tips to help you.
- Even if your loved one is no longer awake, or conscious, they may hear your words. Hearing is the last sense to leave a person who is dying.
- Take the time to say what is in your heart. Sharing your feelings with your loved one may provide you with reassurance and peace after they have died.
- Talking and reminiscing around your loved one, even if they are no longer awake, is another way to connect in a meaningful way during their final days or hours of life.
Oral Care
Oral care, also known as mouth care, is an important part of providing care and comfort during the end of life. Oral care should be provided at least daily, or more often when needed. Oral care involves regular, gentle cleaning of the mouth to maintain comfort and prevent infections. Here are some tips to help. Tips for Providing Oral Care:
- Clean the Teeth and Gums: Gently brush teeth, gums, and the tongue with a soft-bristled toothbrush or sponge applicator moistened with cool water. A small amount of toothpaste may also be used if your loved one can spit out excess toothpaste after oral care.
- Remove Debris: Use oral swabs to remove any pieces of food or other debris from the mouth, when possible.
- Hydrate Mouth for Comfort: Offer sips of water or ice chips if your loved one can swallow or you may use a sponge applicator with a small amount of water to moisten their mouth and lips.
- Lip Care: Apply nonpetroleum based lip balm or mouth moisturizer to prevent cracking and dryness.
Providing a Bed Bath
Providing a bed bath for your loved one allows them to maintain dignity and feel cared for during a vulnerable time. While bed baths help your loved one to be clean and prevent skin breakdown, they can also help provide comfort and alleviate anxiety. The following are tips to providing a safe bed bath.
- Wash your hands and put on gloves (if desired)
- Gather supplies: wash basin with warm water, mild soap, 2-3 washcloths and 2-3 towels
- Make sure as you go, cover exposed body parts not being washed with towels to maintain warmth and dignity
- Wash face with washcloth and dry with a towel
- Wash hands with washcloth and dry with a towel
- Wash arms and legs with washcloth and dry with a towel
- Wash chest/stomach with washcloth and dry with a towel
- Turn onto side and wash back with washcloth and dry with a towel
- Wash private parts last and dry with a towel
- Apply any protective creams as needed to area around private parts
- Apply lotion to rest of the body to maintain healthy skin – may provide hand or foot massage during while doing this
- Use dry or waterless shampoo to clean hair
- Gently comb or brush hair (if desired)
Changing an Adult Diaper or Brief in Bed
The following are tips on how to change an adult diaper or brief while your loved one is in bed. These steps help maintain the dignity and comfort of your loved one while ensuring cleanliness and hygiene.
- Gather supplies: disposable diapers/briefs, wet wipes (or washcloth and warm water)
- Wash hands and put on gloves
- If possible, have your loved one roll onto their side, or lift their hips slightly to access the diaper/brief.
- Unfasten tabs of diaper or tear open sides of pullups at the seams
- Gently pull the front of the diaper/brief down, folding it under the bottom
- Use wipes to clean the private parts, moving from front to back
- Roll up the diaper/brief and place it in a garbage bag
- Slide a clean diaper/brief under your loved one while they are on their side or lifted slightly
- Position the diaper as needed for correct fit
- Bring the front of the clean diaper/brief up between your loved one’s legs and secure the tabs snugly but comfortably
- Remove gloves and wash hands thoroughly
Disease Specific Education
Heart Disease
Heart disease refers to several different conditions in which the heart is not working properly. Some of the most common examples of heart disease are Congestive Heart Failure (CHF/HF), Coronary Artery Disease (CAD), and Cardiomyopathy. Heart disease is serious and can eventually be life-limiting. There are many different causes of heart disease, but many of the symptoms are similar. Patients with advanced heart disease may be eligible to benefit from hospice care when they are experiencing any or all the following symptoms:
- Shortness of breath
- Weight loss
- Weight gain (from edema)
- Edema (Swollen legs/ankles/feet)
- Fatigue
- Loss of appetite/nausea
- Unable to care for self
- Chest pain/tightness
- Dizzy/lightheaded
How Can Hospice Help?
When heart disease progresses into the final or end-stage, symptoms are often more severe and difficult to manage. Hospice can help get these unpleasant symptoms under control such as shortness of breath as well as providing overall comfort. Choosing hospice means your loved one will no longer go to the hospital or receive invasive treatments. They will now be treated in the comfort of home.
For more information, please visit:
Heart Failure: https://www.heart.org/-/media/Files/Health-Topics/Answers-by-Heart/What-Is-Heart-Failure.pdf and https://www.heart.org/en/health-topics/heart-failure Coronary Artery Disease: https://www.heart.org/en/health-topics/consumer-healthcare/what-is-cardiovascular-disease/coronary-artery-disease
Cardiomyopathy: https://www.heart.org/en/health-topics/consumer-healthcare/what-is-cardiovascular-disease/coronary-artery-disease
Alzheimer’s Disease
Alzheimer’s Disease is a brain disorder that slowly destroys memory and thinking skills and, eventually, the ability to carry out the simplest tasks. Advanced Alzheimer’s Disease is considered an end-of-life illness. Other disorders that directly or indirectly affect the brain and are considered end-of-life illnesses as they progress includes Frontotemporal Dementia, Parkinson’s Disease, Huntington’s Disease, and brain injury i.e., stroke or brain aneurysm/bleed. Patients with Alzheimer’s Disease may be eligible to benefit from hospice care when they start experiencing any or all the following symptoms:
- Weight loss.
- Difficulty swallowing or refusing to eat.
- Inability to speak or communicate meaningfully.
- Unable to recognize who they are, where they are, or
the people around them.
- Incontinent of bowel and bladder.
- Not able to care for self and meet personal care needs
- No longer able to walk or transfer self.
- Mood changes such as anxiety and/or agitation
How Can Hospice Help?
When Alzheimer’s Disease progresses into the final or end-stage, symptoms are often more severe and difficult to manage. Hospice can help control these unpleasant symptoms, such as anxiety or agitation, and provide overall comfort. Choosing hospice means your loved one will no longer go to the hospital or receive invasive treatments. They will now be treated in the comfort of home. For more information, please visit: https://www.alz.org/
Liver Disease
Liver disease impacts a person’s ability to digest food, store energy, and remove waste products from the body. There are many types of liver disease, including diseases caused by viruses such as Hepatitis A, Hepatitis B, and Hepatitis C. Liver disease can also be caused by other factors such as alcohol use, certain medications, and poisons. Liver disease can be serious and life-limiting when it reaches the final stage of the disease. Patients with liver disease may be eligible to benefit from hospice care when they start experiencing any or all the following symptoms:
- Swelling of abdomen (ascites) and legs.
- Bruising easily.
- Changes in the color of the stool and urine.
- Jaundice or yellowing of the skin and eyes.
- Weight loss or weight gain if retaining fluid.
- Nausea and/or vomiting.
How Can Hospice Help?
When liver disease progresses into the final or end-stage, symptoms are often more severe and difficult to manage. Hospice can help get these unpleasant symptoms under control such as swelling of the abdomen and legs as well as providing overall comfort. Choosing hospice means your loved one will no longer go to the hospital or receive invasive treatments. They will now be treated in the comfort of home. For more information, please visit: https://liverfoundation.org/
Cancer
Cancer is a disease caused by the rapid growth of abnormal cells that develop beyond their usual boundaries and invade other parts of the body including other organs. The spread of cancer to other organs is known as metastasis and is the primary cause of death from cancer. Some of the most common primary sites of cancers are breast, lung, colon, prostate, ovarian, skin, pancreas, and stomach. While some cancers can be successfully treated, others can be more serious and eventually life-limiting. Patients with advanced stages of cancer may be eligible to benefit from hospice when treatment is no longer effective and/or the burden of treatment outweighs the potential benefits. Some of the symptoms commonly experienced with cancer includes the following:
- Weight loss
- Pain
- Shortness of breath or feeling breathless
- Swelling in the feet, legs, or hands
- Fatigue
- Loss of appetite/nausea
- Change in bowel habits
- Skin changes such as new sores that will not heal
How Can Hospice Help?
When cancer progresses into the final or end-stage, symptoms are often more severe and difficult to manage. Hospice can help get these unpleasant symptoms under control such as pain or shortness of breath as well as providing overall comfort. Choosing hospice means your loved one will no longer go to the hospital or receive invasive treatments. They will now be treated in the comfort of home. For more information, please visit: https://www.cancer.org/
Lung Disease
Lung disease refers to many different diseases or disorders that prevent the lungs from working properly. Some of the most common lung diseases are: Patients with Lung Disease may be eligible to benefit from hospice care when they start experiencing any or all the following symptoms:
- COPD (Chronic Obstructive Pulmonary Disease)
- Chronic Bronchitis
- Chronic Asthma
- Bronchiectasis
- Lung Cancer
- Emphysema
- Pulmonary Fibrosis
- End-Stage Tuberculosis
- Pulmonary Hypertension
- Sarcoidosis
Patients with Lung Disease may be eligible to benefit from hospice care when they start experiencing any or all the following symptoms:
- Shortness of Breath
- Changes in Mucus Production
- Fevers
- Weight Loss/Loss of Appetite
- Edema
- Worsening Cough
- Fatigue/Tired
- Chest Pain/Tightness
- Dizziness
- Poor Sleep
How Can Hospice Help?
When lung disease progresses into the final or end-stage, symptoms are often more severe and difficult to manage. Hospice can help get these unpleasant symptoms under control such as shortness of breath as well as providing overall comfort. Choosing hospice means your loved one will no longer go to the hospital or receive invasive treatments. They will now be treated in the comfort of home. For more information, please visit https://www.hospiceinnovations.org/for-patients-families/advanced-lung-care-handbook/
Neurological Diseases
Neurological diseases impact a person’s nervous system, which includes the brain, spinal cord, nerves, and muscles. Some examples of neurological diseases are Parkinson’s disease, Stroke, Amyotrophic Lateral Sclerosis (ALS), Multiple Sclerosis (MS), Lewy Body Dementia, and Huntington’s Disease. These are all serious, life-limiting conditions that can lead to permanent decline of the nervous system. Patients with neurological diseases may be eligible to benefit from hospice care when they start experiencing any or of the following symptoms:
- Weight loss.
- Nagging cough.
- Shortness of breath.
- Difficulty swallowing.
- Difficulty speaking or softening of the voice.
- Unable to care for self or meet personal care needs.
- Unable to walk or transfer self.
- Incontinent of bowel and bladder.
How Can Hospice Help?
When a neurological disease progresses into the final or end-stage, symptoms are often more severe and difficult to manage. Hospice can help get these unpleasant symptoms under control such as shortness of breath as well as providing overall comfort. Choosing hospice means your loved one will no longer go to the hospital or receive invasive treatments. They will now be treated in the comfort of home.
For more information, please visit:
ALS: https://www.als.org/understanding-als
Parkinsons: https://www.michaeljfox.org/parkinsons-101
Stroke: https://www.stroke.org/en/about-stroke
Multiple Sclerosis: https://mymsaa.org/ms-information/overview/introduction/
Huntington’s Disease: https://hdsa.org/what-is-hd/overview-of-huntingtons-disease/
Chronic Kidney Disease
Chronic Kidney Disease (CKD) is a term used to describe the gradual loss of function of a person’s kidneys. Kidneys play an important role in filtering waste and fluids from the body, which are then eliminated in a person’s urine. When the kidneys are diseased and unable to eliminate this waste, dangerous levels of fluid, electrolytes, and waste can build up in your body. As CKD progresses to the most serious and final stage, treatment options are limited, and the burden of treatment often outweighs the benefits. Patients with Chronic Kidney Disease may be eligible to benefit from hospice care when they start experiencing any or all the following symptoms:
- Weight loss or weight gain from retaining fluid
- Loss of appetite
- Changes in the amount of urine produced usually low to none
- Nausea and vomiting
- Fatigue and weakness
- Sleep problems either unable to sleep or sleeping all the time
- Decreased mental sharpness and/or confusion
- Muscle twitching and cramps
How Can Hospice Help?
When kidney disease progresses into the final or end-stage, symptoms are often more severe and difficult to manage. Hospice can help get these unpleasant symptoms under control such as nausea and vomiting as well as providing overall comfort. Choosing hospice means your loved one will no longer go to the hospital or receive invasive treatments. They will now be treated in the comfort of home.
For more information, please visit: https://www.kidney.org/atoz/content/about-chronic-kidney-disease
Common Symptoms/What to Expect Near End of Life
Breathing Changes
Breathing changes are common at the end of life. There may be changes in how deep your loved one’s breaths are, how often they take a breath, and/or the pattern of their breathing; all of which are normal changes.
- When patients have moisture, or saliva, at the back of their throat and they are unable to cough or clear the saliva, it makes a “wet” or rattling sound when they breathe. This may sound upsetting, but it rarely causes any discomfort or distress to your loved one.
- Breathing may alternate between being rapid to being slow, shallow, and deep.
- Your loved one may start to breathe with their mouth open as they are dying. This is common and normal even for people who have never been mouth breathers.
- Your loved one may have long pauses between breaths, which are known as periods of “apnea.” These pauses may last for a few seconds up to a minute. As your loved one gets closer to the end of their life, these pauses may become longer.
- Most people have an irregular pattern of breathing in the minutes leading up to death. This is often followed by a brief period of very shallow breaths, before breathing eventually stops and death occurs.
Changes in Bladder and Bowel Function
It is common to have changes in bladder and bowel function as the body goes through the natural process of decline. Here are some of the typical changes that may occur:
- Constipation: This can be caused by a decrease in the intake of food and fluids, a reduction in physical activity, and as a side effect of some medications. It may also be related to the bowel muscles becoming less effective at moving stool.
- Diarrhea: This may occur due to the reduced absorption of fluid into the body’s digestive system. It may also be a side effect of certain medications and/or the body’s inability to process food properly.
- Incontinence: This may occur as the muscles that control bladder and bowel function gradually weaken. It may also occur when your loved one is less awake and/or alert, and therefore unaware of their bowel and bladder functions.
- Reduced urinary output and/or reduced bowel movements: This occurs as food and fluid intake decreases resulting in less waste being produced which then causes less to no urine output and/or fewer bowel movements. Urine may also appear darker in color.
- Urinary retention: This occurs when the bladder is not emptying completely, which can lead to discomfort and risk of infection. Placing a tube called a Foley catheter into the bladder can help empty the bladder and provides comfort.
*If your loved one experiences any of the above symptoms, please let the hospice nurse know so we may assist in keeping your loved one comfortable and to prevent any complications.
Decreased Appetite
Food and nutrition are often seen as a way of providing love. As the end of life nears, it is often very difficult for caregivers to understand or accept their loved one no longer wants or even enjoys foods like they once did.
- It is common for people nearing the end of life to lose their appetite or desire to drink fluids.
- Food and drinks your loved one once enjoyed may no longer taste good.
- It is important to let your loved one decide when he/she wants to eat and drink. Support their decision by letting them know it’s okay to say “no” to food.
- Offer small bites and sips often, but do not pressure your loved one to eat or drink. Focus on small amounts of easy-to-swallow foods and drinks.
- Provide oral care often as this provides comfort and it may help make food taste better.
- As the body’s functions slow down, food is no longer able to be processed. This can cause nausea, vomiting, or even choking if eating is forced.
- Your loved one should always be awake and alert to accept any food or fluids to prevent choking.
Depression
Feelings of grief and sadness often accompany facing the reality of a terminal, or life-limiting diagnosis. These feelings are normal and expected. For many people facing a terminal diagnosis, these normal feelings can evolve into depression.
Signs and Symptoms of Depression
- Mood changes such as sadness, anxiety, feelings of guilt, hopelessness.
- Loss of interest in activities your loved one usually enjoys.
- Changes in sleep patterns such as inability to fall asleep, sleeping too much, sleeping too little, and/or restless sleep.
- Changes in appetite such as loss of appetite or little interest in eating.
- Changes in weight such as weight loss or weight gain.
- Changes in behavior such as crying, irritability, and agitation.
- Changes in thinking such as inability to concentrate, and/or thoughts of suicide.
It is important to recognize when sadness and grief become something more serious. Depression, even in the terminally ill, is treatable. Many symptoms of depression can be like the symptoms of terminal illness, so it is important to talk to your hospice nurse about your concerns. Talking through concerns with a social worker or chaplain can also provide much needed support.
End of Life Confusion
End of life confusion, also known as delirium, may occur as the brain is in the natural shutdown process of dying. This process changes the person’s ability to process thoughts.
Signs and Symptoms of Confusion/Delirium:
- Confusion/disorientation
- Changing levels of consciousness and alertness
- Impaired thoughts and/or inability to focus
- Memory changes i.e., forgetfulness
- Agitation or restlessness
- Hallucinations or delusions
- Anxiety or fearfulness
- Mood changes i.e., irritability
- Insomnia, difficulty falling asleep and/or staying asleep
- Decreased ability to communicate effectively and clearly
End of life confusion can be a distressing part of the dying process, however, there are medications and other interventions that can ease these distressing symptoms. Talk to your hospice nurse about how to best manage these symptoms.
Fatigue and Sleep
At the end of life, people spend more hours of the day sleeping than they do being awake. It is also normal for people to feel very fatigued and weak, and to need help with even the simplest tasks.
- It is easy to be discouraged by seeing your loved one sleep so much, but it is important to remember that this is a natural part of the dying process.
- When your loved one is awake, offer to assist them with tasks to help conserve their energy.
- You can provide comfort to your loved one while they are sleeping through gentle touch, holding hands, or just sitting at their bedside.
- As the end of life draws near, your loved one may gradually become less and less responsive when spoken to or touched and eventually can transition into being totally unresponsive. This is a common and a normal part of the dying process.
Fevers
Fevers at the end of life are very common and may be managed with medications, such as Tylenol, or other comfort-focused measures. A few of the most common reasons fevers occur are:
- Dehydration: As the body goes through the natural shut-down process, dehydration is common and can cause the body temperature to rise.
- Neurological Decline: The hypothalamus, which is the part of the brain that regulates body temperature, becomes less effective at maintaining a normal body temperature.
- Infection: The ability to fight infection weakens as the body shuts down, making people more vulnerable to infections and fevers.
Beyond medications, there are other many other comfort-focused measures that can help manage the discomfort associated with fevers. Here are some of the most effective fever management measures:
- Apply a cool, damp cloth to the forehead, neck and wrists.
- Use fans to circulate the air and help cool your loved one.
- Use lightweight bedding and sheets.
- Adjust the room temperature.
Nausea and Vomiting
Nausea is an uncomfortable feeling in your stomach that makes you feel like you could throw up. Vomiting is simply your body’s own natural way of emptying the contents of your stomach. Nausea and vomiting can have many different causes such illness, motion, side effects of medications, constipation, excessive coughing, and certain foods and smells.
Tips For Managing Nausea/Vomiting
- Suck on ice chips
- Sip on ginger ale or other clear liquids
- Eat small, frequent meals
- Eat foods that are room temperature or cooler
- Sit up during and after eating – at least for 1-2 hours
- Do not force eating
- Keep saltine crackers at the bedside
- Avoid strong odors
- Keep room at a comfortable temperature
- Use a fan to circulate air in the room
- Apply a cool, damp cloth to forehead or back of neck
- Rinse your mouth out after vomiting
- Clean your mouth before and after eating
- Wear loose-fitting clothing
Let your hospice nurse know if you are experiencing nausea or vomiting. Your hospice nurse will discuss other options to manage these distressing symptoms such as medications and/or holistic therapies like aromatherapy.
Oral Secretions
An increase in oral secretions or saliva in the back of the throat is normal for people who are dying. This occurs because people have a decrease in the ability to cough or clear secretions at the end of life. Here are some tips to help manage your loved one’s secretions.
- Medications may be used to assist with drying up secretions, however, they may not be the best answer. Your hospice nurse can provide more information about this option.
- Placing your loved one on their side or tipping their head to the side will help to drain the saliva out of the side of their mouth. Make sure to place a washcloth or towel under the side of their head to absorb the saliva.
- Raising the head of the bed slightly may help to drain or clear the saliva from the back of the throat.
- Suctioning has limited benefits, as it can eventually make the secretions increase.
- It is important to remember when your loved one has “wet” or rattling breathing, they are not experiencing any distress or discomfort. This is a natural part of dying and is more distressing for others to hear than it is for your loved one.
Pain
Pain is the experience of feeling discomfort or suffering. Pain can be a physical sensation, such as achiness, cramps, or even pressure. Pain can also be an emotional experience and can include feelings of fear, anxiety, and distress. However pain is felt, it is unique to the person experiencing it.
Your hospice team can help you manage your pain. To treat pain in the most effective way, the team will ask questions to better understand your pain, such as:
- How bad or intense is the pain?
- Where is the pain?
- Is the pain new?
- How would you describe the pain?
- Does the pain keep you from your normal activities?
- What makes the pain better?
- What makes the pain worse?
- How well is the current medication for pain working?
- Are you having any side effects related to your pain or the pain medication being used?
There are many options available to manage pain. Your hospice team will work with you to determine the best treatment options and to develop a plan to help get relief from both your physical and emotional pain.
Shortness of Breath
“Shortness of breath” is a term used to describe the feeling of being out of breath or not getting enough air when you breathe. It may also feel like you are unable to take a deep enough breath.
What Causes Shortness of Breath?
- Diseases such as cancer, heart disease, or lung disease.
- Anxiety can make you feel short of breath, and shortness of breath can make you feel anxious.
- Exercise or exertion.
- Excessive coughing.
- Body positions that restrict breathing such as poor posture, lying flat on your back, or sleeping on your stomach.
- Increased secretions in the airway.
- Warm, humid weather.
What Can Help Relieve Shortness of Breath?
- Medications such as opioids i.e., Morphine, steroids, nebulizers, and oxygen can all be used to treat shortness of breath.
- Conserve your energy and take frequent breaks to rest.
- Adjust your body position such as lying on your side if able to make breathing easier.
- Try pursing your lips to breathe.
- Adjust your environment to be comfortable and/or utilizing a fan.
- Relax and meditate.
- Know your individual triggers and avoid them when possible.
Let your hospice nurse know if you are experiencing symptoms of shortness of breath. Your team will discuss options to help you manage this distressing symptom, such as medications and/or other interventions.
Skin Temperature and Color Changes
Changes in skin color and temperature are common at the end of life and are usually a sign of the body’s natural shutdown process.
Common Skin Color Changes are:
- Pale skin (Pallor): The skin may appear to be white, lighter than usual, or very ashen. This may be seen throughout the body, or in smaller areas such as the face, hands, and feet.
- Blue-tinged skin (Cyanosis): This is common to see on the lips, inside the mouth, and on the fingernails and/or toenails.
- Blotchy, purplish-red discoloration (Mottling): This is usually seen on the feet and legs, but other areas of the body may have mottling as well.
Common Skin Temperature Changes are:
- Decreased Body Temperature: This may be felt as skin that is cool/cold to the touch effecting the entire body or effecting only smaller areas such as the extremities (legs, feet, hands).
- Intermittent Fevers: This occurs when the body temperature rises above the normal range. Fever episodes may be short, last for several hours, or days. Common symptoms include sweating, chills, and general discomfort. If this occurs, your hospice nurse can advise you on medications, or other measures, that are available to provide comfort.
Symbolic Language/Near Death Awareness
At end of life, the person who is dying may have an awareness death is near. They may use words or talk in a way that may be confusing to others, but it often has meaning for the dying person. This is a very normal and common occurrence at the end of life.
Common Symbolic Language/Near Death Awareness Experiences:
- Your loved one may talk about events from the past. They may also “see” or “talk” to people who have already died.
- Your loved one may talk about leaving or going to another place.
- Your loved one may express the desire to talk about their life and reminisce.
- Your loved one may express the need for forgiveness from others.
Tips for the Caregiver:
- Offer support and be present.
- Pay attention to what your loved one is saying. This may be symbolic of the life they led.
- Being with and watching over your loved one as they near death can be distressing. However, this can also be a very meaningful time letting your loved one know how much you care, and they are not alone.
- “Seeing” or “talking to” loved ones who have already died often provides comfort to the person who is dying.
Terminal Restlessness
Terminal restlessness, also known as terminal agitation, is a state of physical and emotional agitation or distress commonly experienced by patients nearing the end of life. It may occur as the brain is in the natural shutdown process of dying.
Common Symptoms of Terminal Restlessness:
- Agitation or restlessness, unable to sit still
- Confusion or disorientation
- Anxiety
- Involuntary movements or twitching
- Hallucinations or delusions
- Insomnia or restless sleeping
- Moaning, calling out, or yelling
- Attempting to get out of bed repeatedly
- Picking at blanket/clothing
- Resistance to care
Terminal restlessness can be an upsetting part of the dying process, however, there are medications and other interventions that can ease these distressing symptoms. Talk to your hospice nurse about how to best manage these symptoms.
Withdrawal
As a person nears death, they will usually become less “present” and interactive with the people around them. This withdrawal from the world, including family and friends, is a natural part of the dying process. Here are some tips as your loved one withdraws.
- Watching a loved one withdraw can be difficult. Providing a calm and supportive environment is the best way to care for your loved one during this time.
- When a person starts to withdraw from their physical surroundings, it is thought to be a time that they may be reflecting and processing the emotional and spiritual aspects of dying. Providing a quiet calm environment and being present is the best way to support your loved one during this time.
Medications and Comfort Focused Treatments
Aromatherapy
It is well known that certain smells can have a powerful effect on the brain, and therefore the body as well. Aromatherapy involves essential oils (lavender, peppermint, etc.), which help improve a patient’s physical, emotional and spiritual well-being.
Some of the many benefits of aromatherapy are:
- Improves nausea
- Helps control pain
- Reduces anxiety and agitation
- Creates a calm and peaceful environment
- Improves sleep
- Promotes relaxation
Benefits of Integrative Therapies
While medications are often used to treat pain and other common symptoms at end-of-life, integrative therapies such as music therapy, aromatherapy, massage therapy, and pet therapy can also be used to improve symptoms and quality of life.
Some of the many benefits of integrative therapies are:
- Eases symptoms, such as: pain, restlessness, nausea, agitation.
- Decreases anxiety and depression.
- Increases feelings of well-being and comfort.
- Promotes communication and socialization.
- Fosters meaningful sensory experiences.
- Creates positive memories at end-of-life.
- Helps with expression of emotion.
- Improves overall comfort and quality of life.
- Provides relaxation.
Comfort Medications Myths
MYTH: “Everyone on hospice ends up on Morphine, which causes people to die sooner.”
FACT: While the use of Morphine is common in hospice, there are also many other non-opioid medications used to keep you comfortable. Morphine may be needed if these medications are not effective enough by themselves. Morphine is a very effective medication for easing pain and shortness of breath, which are both common symptoms at end-of-life. Morphine does NOT cause death or make it happen any sooner. Morphine simply makes end-of-life more comfortable.
MYTH: “If my loved one takes Morphine, he/she will become addicted to it.”
FACT: Someone who is dealing with a terminal illness and is experiencing pain and/or shortness of breath does not typically form an addiction to Morphine or any other opioids. The benefits of Morphine greatly outweigh any unpleasant side effects such as increased sleepiness, nausea, or itching which usually clear up within days of starting these medications.
Increasing a patient’s comfort and enhancing quality of life are the main goals of hospice care. One of the most important comfort measures hospices provide is through the use of different medications – all aimed at relieving common end-of-life symptoms such as pain, shortness of breath, anxiety, and nausea.
The following is a list of the most commonly used comfort-focused medications in hospice care, the symptoms they treat, and how they are administered.
- Acetaminophen (Tylenol)
Purpose: Acetaminophen is a very commonly used hospice medication. It can be given by mouth (as a pill or tablet) or as a rectal suppository. Acetaminophen is gentle on the stomach and tolerated well by most people. It is commonly prescribed for mild to moderate pain, general discomfort, headaches, and fevers. It can also be used alongside stronger pain medications to help reduce overall pain without increasing sedation.
Possible Side Effects: May cause nausea.
- Morphine (Roxanol)
Purpose: Morphine is one of the most widely used medications in hospice. It helps manage moderate to severe pain and can also ease shortness of breath, both of which are common symptoms near the end of life. It is usually given by mouth or sublingually (under the tongue).
Possible Side Effects: May cause drowsiness, constipation, nausea, and/or itching. ** It is important to talk to your hospice provider about these possible side effects, as most are temporary and can be prevented.
Important considerations:
- Side effects typically decrease after 2-3 days and can be managed with other medications or interventions, if needed.
- Morphine does NOT cause death to happen sooner. This is a common misconception about this medication.
- Addiction is rare when used to treat symptoms.
- The dose can be increased safely as needed to effectively manage pain and/or shortness of breath symptoms.
- Pain is best managed before it becomes severe. “Staying ahead” of pain is the best way to manage it effectively.
- Hydromorphone (Dilaudid)
Purpose: Hydromorphone is another powerful opioid, similar to morphine, but often used when morphine isn’t well-tolerated or effective. It is typically used for moderate to severe pain and can also ease shortness of breath, both of which are common symptoms near the end of life. It is usually given by mouth or sublingually (under the tongue).
Possible Side Effects: May cause drowsiness, constipation, nausea, and/or itching. ** It is important to talk to your hospice provider about these possible side effects, as most are temporary and can be prevented.
Important considerations:
- Side effects typically decrease after 2-3 days and can be managed with other medications or interventions, if needed.
- Hydromorphine does NOT cause death to happen sooner. This is a common misconception about this medication.
- Addiction is rare when used to treat symptoms.
- The dose can be increased safely as needed to effectively manage pain and/or shortness of breath symptoms.
- Pain is best managed before it becomes severe. “Staying ahead” of pain is the best way to manage it effectively.
- Lorazepam (Ativan)
Purpose: Lorazepam is a medication that is commonly used to help calm anxiety, agitation, and restlessness. It is also effective in easing shortness of breath. It is usually given by mouth or sublingually (under the tongue).
Possible Side Effects: May cause drowsiness.
- Haloperidol (Haldol)
Purpose: Haloperidol is a medication commonly used in hospice to treat agitation and restlessness. It is also effective for managing nausea. It is usually given by mouth or sublingually (under the tongue).
Possible Side Effects: May cause drowsiness, dry mouth, and/or constipation. ** It is important to talk to your hospice provider about these possible side effects, as most are temporary and can be prevented.
- Bisacodyl (Dulcolax)
Purpose: Bisacodyl is a medication commonly used in hospice to prevent and/or treat constipation. Bisacodyl is a stimulant laxative that helps keep bowel movements regular and comfortable. It is usually given by mouth or as a rectal suppository.
Possible Side Effects: May cause abdominal cramping and/ or diarrhea.
How to Administer Medications
Taking medications or providing medications to your loved one is an important job. Your hospice nurse will provide you with detailed instructions regarding all medications that might be used to provide comfort and manage symptoms. Medications can be given in a variety of ways. The following is a list of the most common ways to administer medications.
By mouth (oral) – Oral medications can be in the form of pills, capsules, or liquids. Most pills and capsules can be swallowed with water or other liquids. The best way to take pills or capsules by mouth is to sit upright, place medication on tongue, drink a small amount of fluid, and swallow. Liquid medications can be given by using a syringe or a medication measuring cup.
Inside cheek (buccal) – Some liquid medications are given inside the mouth by the side or inner lining of the cheek called the buccal mucosa. This is used when a person has difficulty swallowing or they are not awake enough to swallow safely. A syringe is usually used to administer liquid medication into the buccal mucosa.
Under the tongue (sublingual) – This can be used with pills or tablets that dissolve. Dissolving pills can be placed under the tongue, and they will “melt” or absorb within a brief period. Liquids given under the tongue will usually be administered by a syringe.
Rectal route – This route may be used for certain medications typically in the form of a suppository especially if taking medications by mouth is difficult or unsafe. The person will be laying down in a comfortable position on their left side. The medication or suppository is inserted into the rectum. Your hospice nurse will instruct you on how to do this safely and properly.
Skin (transdermal) – This is typically in the form of a patch or cream. Follow the directions for each specific medication, as the site where to apply on the body may differ. Make sure the skin is clean and dry when applying a cream or patch.
By inhalation (can be through mouth or nose) – This can be in the form of oxygen being delivered through a nasal canula (through the nose) or a mask (over the mouth). This can also be a nebulizer treatment, which provides medications inhaled through a mouthpiece. There are special precautions that need to be in place with oxygen. Your hospice nurse will instruct you on how to use this safely and properly.
How to Crush Medications
Ask your hospice nurse before using this method, because some medications should not be crushed.
- Wash your hands with soap and water or use hand sanitizer. Try not to touch the medication with your bare hands, wear gloves, if possible.
- To crush the medication, use either a pill crusher or the back of a metal spoon and a small bowl.
- Crush the medication, then put all the contents into a small bowl or cup.
- Draw up 0.5 to 2 mL (milliliters) of water into your syringe. If it is difficult for the patient to swallow, use the smaller amount.
- Add the water from the syringe to the crushed medication in the bowl. Mix the crushed medication and water together until the medication is dissolved.
- Draw up the dissolved mixture into the syringe. With the tip of the syringe in the mixture, pull up slowly on the plunger to “draw up” the liquid.
- Have the person sit up or raise the head of the bed up to at least a 30-degree angle.
- Slowly dispense all the dissolved medication into the mouth on the tongue (if they are awake and can swallow), under the tongue, or in the side of the mouth/cheek. Check with your hospice nurse on the best route for administering medication.
How to Dispose of Unused Medications
When medications are no longer needed or being used, it is important to consider how to dispose of or get rid of them in a safe way. While hospice team members are not able to take medications out of the home for you, they can assist you with finding a safe way to dispose of medications that are no longer needed.
To dispose of medications in your household trash:
- Remove medications from their original container and mix them with undesirable substances such as coffee grounds, cat litter, or even dirt. If you have liquid medications, these can be poured out into an unused depends to be absorbed.
- Put the mixture or depends into a sealed container (zip lock bag, tied up plastic grocery bag, etc.).
- Throw sealed container into the garbage.
There are many local medication disposal sites that are available. For a list of medication disposal sites in Illinois, please visit:
How to Draw up Liquid Medications with a Syringe
Liquid medications are often given with an oral syringe. An oral syringe has specific measurement lines that are used to ensure the right amount, or dose, of medication is being “drawn up” into the syringe. The steps for using an oral syringe are as follows:
- Wash your hands. Make sure you have the right medication bottle.
- Gently roll the medication bottle between your hands to ensure the medication is mixed well.
- Remove the cap from the bottle. Insert the bottle syringe adapter, if available.
- Insert the tip of the oral syringe into the syringe adapter.
- If using a syringe adapter, turn the bottle upside down and gently pull the plunger of the syringe until the medication reaches the correct amount. The top of the plunger should be at the measurement line to draw up the correct dose.
- If you aren’t using a syringe adapter, hold the bottle in your hand or place it on a table. Insert the tip of the oral syringe into the bottle and gently pull up the plunger to the appropriate measurement line.
- Turn the syringe so the tip is pointing toward the ceiling.
- Tap the syringe to move the air bubbles to the top of the syringe.
- Slowly push the plunger until any big air bubbles are gone. The top of the plunger should be at the correct measurement line.
Music Therapy
Music can improve quality of life and a person’s overall sense of well-being. Music therapy benefits not only the person but also their families and caregivers.
Some of the many benefits of music therapy are:
- Promotes pain relief.
- Promotes relaxation.
- Helps with expression of emotions.
- Increases feelings of meaning and purpose.
- Improves comfort.
- Increases feelings of closeness and acceptance.
- Promotes an environment to help resolve family conflict and stress.
- Promotes a sense of spiritual support.
- Fosters meaningful sensory experiences.
- Creates positive memories at the end of life.
Pet Therapy
Pet therapy involves the use of trained animals, usually dogs, to provide comfort, companionship, and emotional support to patients with serious or life-limiting illnesses. Pet therapy has been shown to have many benefits for persons at end-of-life.
Some of the many benefits of pet therapy are:
- Provides pain relief.
- Reduces anxiety and depression.
- Promotes relaxation.
- Promotes overall improvement in mood and emotional well-being.
- Reduces feelings of isolation and loneliness.
- Encourages communication and socialization.
- Provides joy and comfort.
- Reduces emotional stress.
Caring for Someone with Dementia
Understanding Anger and Aggression
Dementia affects the brain’s ability to process information, communicate, and manage emotions. A person with dementia may lash out because they feel scared, confused, or unable to express their needs. Triggers may include physical discomfort, overstimulation, unmet needs (like hunger or pain), or even unfamiliar environments. These moments can feel overwhelming and even hurtful, especially when directed at the person who loves them and takes care of them. It is important to remember that these behaviors are not intentional, they are simply symptoms of the disease.
Tips for Caregivers
- Use Gentle Communication: Speak softly, keep sentences short, and use a reassuring tone rather than reasoning or arguing.
- Offer Comfort and Redirect: Suggest a walk, move to a quieter environment, ask the person for help with a task, offer the person something to hold or touch, or ask questions about a family photo – these are all different ideas to facilitate redirecting them away from whatever was causing the behavior(s). Sensory experiences are often successful at shifting focus away from distress.
- Address Triggers: Make sure any possible triggers are addressed, such as hunger, pain or discomfort, overstimulation, or needing to use the bathroom.
- Respect Personal Space: Step back slightly if the person is agitated; this shows safety and avoids escalation.
- Identify Triggers and/or Patterns: Keep a journal of when outbursts occur. You may discover triggers like loud noises, crowded rooms, or certain times of day. Was the person tired, overwhelmed, or in pain? Addressing the underlying cause can prevent future episodes.
- Take Care of Yourself – Managing aggression can be exhausting. Lean on support groups, respite care, and family or friends so you don’t carry the burden alone.
Final Thoughts
Anger and aggression in dementia are not your loved one’s fault — or yours. They are symptoms of the illness. With patience, compassion, and practical strategies, caregivers can create a calmer environment while protecting their own well-being.
Understanding Anxiety and Agitation
Anxiety and agitation are common behaviors that can appear as the brain struggles to process the world. Your loved one may pace, fidget, ask repeated questions, or seem restless. These behaviors are not deliberate; they are signals that something feels overwhelming or unsafe to them. Loud noises, unfamiliar surroundings, fatigue, or even too many choices can create distress. Sometimes agitation stems from physical discomfort such as pain, hunger, or needing the restroom.
Tips for Caregivers
- Stay Calm and Reassuring: Use a gentle voice, steady eye contact, and relaxed body language. Your calmness can help reduce their fear.
- Simplify the Environment: Limit clutter, noise, or overstimulation. A quiet, familiar space often brings comfort.
- Offer Comfort and Routine: Predictable schedules and familiar activities provide a sense of security.
- Redirect with Purpose: Engage the person in soothing activities like folding laundry, listening to music, or taking a short walk.
- Address Triggers and Check for Basic Needs: Sometimes a snack, a drink of water, or using the bathroom is all that’s needed to ease agitation.
Final Thoughts
It is important to remember that anxiety and agitation are a behaviors associated with dementia — not a reflection of who the person is or who you are as a caregiver. By approaching these moments with patience and compassion, you can bring comfort and help them feel safe.
Understanding Hallucinations
Hallucinations occur when changes in the brain alter how sights and sounds are processed. They are often linked to changes in the brain caused by dementia. They may also be triggered by poor lighting, infections, medication side effects, or fatigue. Your loved one may see people, animals, or objects that aren’t present, or hear voices or other noises that don’t exist. Hallucinations can be unsettling for both the person experiencing them as well as for the caregivers who witness them.
Tips for Caregivers
- Stay Calm and Reassuring: Instead of telling your loved one that what they see or hear isn’t real, acknowledge their feelings: “That sounds scary, but you’re safe here.” Dismissing or arguing about their experience can increase distress.
- Adjust the Environment: Reduce shadows, improve lighting, and remove distracting patterns or mirrors that may cause confusion.
- Redirect Gently: Shift focus with a soothing activity: play calming music, look through a photo album, give them a comforting object, or involve them in a simple task like folding laundry.
- Assess Triggers: Keep notes on when hallucinations occur. Report patterns to healthcare providers, as hallucinations may be worsened by infections, dehydration, or medication side effects.
- Encourage Routine and Predictability: Structured daily activities reduce anxiety, which may lessen hallucinations.
- Prioritize Safety: If hallucinations cause unsafe behaviors, gently redirect them to a safe space and remove any potential hazards.
Final Thoughts
When hallucinations occur, it is important to remember that they can feel very real and even frightening to the person experiencing them. By staying calm and offering gentle reassurance, you can provide a sense of safety that can help ease the fear that often accompanies the hallucinations.
Understanding Depression in Dementia
As dementia progresses, the brain changes in ways that affect mood, motivation, and emotions. Feelings of loss, confusion, or frustration may contribute to sadness. Social isolation, pain, or lack of stimulation can also play a role. These changes can be difficult to see — but understanding what’s happening and how to respond can make a difference.
Tips for Caregivers
- Encourage Connection: Gently involve your loved one in social interactions, even brief visits with friends, family, or support groups.
- Maintain Routine: Familiar daily schedules provide stability and reduce stress.
- Promote Enjoyable Activities: Focus on simple, meaningful tasks—listening to music, looking through photos, gardening, or short walks.
- Offer Emotional Support: Sit with them, hold their hand, and use reassuring words. Sometimes quiet companionship is the most powerful comfort.
- Involve Medical Professionals: Talk with your healthcare team if you notice signs of depression. There are treatments available - such as medications and therapy.
Final Thoughts
Depression can be difficult for both the person with dementia and the caregiver. It’s important to remember there are effective treatments available. By seeking help when needed and practicing self-care, you’ll be better able to provide the support your loved one needs.
Understanding Repetition
One of the most common — and often most frustrating — behaviors caregivers experience in someone with dementia is repetition. This might come in the form of asking the same question over and over, telling the same story repeatedly, or performing the same action multiple times a day. While it can be challenging to manage, repetition is a symptom of the disease, not a deliberate act.
Repetition in dementia often stems from memory loss and confusion. A person may not remember asking a question five minutes ago, or they may lose track of recent conversations entirely. Repeating stories or actions can also be a source of comfort when the world around them feels unpredictable or unfamiliar. In some cases, repetition can be a signal that the person is feeling anxious, bored, or uncertain, and it is their way of expressing these emotions.
Tips for Caregivers
- Stay Calm and Patient
Reassure yourself that the repetition is not intentional. Getting frustrated won’t help them — or you. Take a deep breath before responding. - Gently Redirect
If a question keeps coming up, answer it calmly and try to shift their attention to a different activity, like looking at a photo album or taking a short walk. - Provide Reassurance
Often, repetition comes from a need for reassurance. Simple, soothing responses — “You’re safe here,” or “Everything is okay” — can ease their anxiety. - Look for Patterns
Notice when and where repetition happens. Are they more repetitive in the evening? When they’re tired or hungry? Understanding the pattern can help you anticipate and reduce triggers. - Use Visual Aids
For frequently asked questions — like “What day is it?” or “When are we eating?” — consider placing a whiteboard or a calendar in a visible area as a helpful reference.
Final Thoughts
Repetition can wear on even the most compassionate caregiver. Make sure to take regular breaks, seek support and accept help from family and/or friends, and prioritize your own well-being. You’re doing incredibly important — and difficult — work.
While repetition is a hallmark of dementia, it’s also an opportunity to practice patience, compassion, and creativity. Every repeated question is a chance to connect, to comfort, and to understand what your loved one might be feeling beneath the surface. They may not remember the question — but they will remember how you made them feel.
Understanding Sleep Issues and Sundowning
Caring for someone with dementia often means navigating challenging behaviors — and sleep disturbances are among the most exhausting. Many caregivers notice their loved one becomes more restless, confused, or agitated in the late afternoon or evening. This phenomenon, known as sundowning, can make nights especially difficult. Some of the most common sleep problems include trouble falling asleep, frequent waking during the night, and excessive daytime sleepiness or napping.
There’s no single cause for sleep issues and sundowning, but possible reasons include changes in the brain’s internal clock, reduced lighting and increased shadows in the evening, fatigue from the day’s activities, unmet needs like hunger, pain, or needing the bathroom, and/or disrupted sleep-wake cycles.
Tips for Caregivers
- Stick to a Routine
A consistent daily schedule helps reduce confusion. Keep wake-up times, meals, and bedtimes the same every day. - Maximize Daytime Light
Exposure to natural sunlight during the day can help reset the body’s internal clock. - Limit Stimulants
Avoid caffeine, sugar, and heavy meals in the late afternoon and evening. - Create a Calm Evening Environment
Reduce noise, avoid overstimulation, and keep things quiet and predictable. Calming music, a warm blanket, or a favorite activity can help ease the transition to bedtime. - Encourage Gentle Activity During the Day
Too much daytime napping or inactivity can make nighttime rest harder. A short walk or simple activity can help use up excess energy. - Reassure, Don’t Argue
If confusion or agitation arises, stay calm. Offer reassurance and redirect rather than trying to explain or correct. - Ensure Safety at Night
Install nightlights, remove trip hazards, and consider motion sensors or monitors if wandering is a concern.
Final Thoughts
Sundowning and sleep issues can disrupt your own rest and lead to caregiver burnout. Whenever possible, ask for help from family, friends, respite care services, and/or support groups. Understanding why these behaviors happen — and what you can do — can make a big difference for both you and the person you’re caring for.
Understanding Suspicion and Delusions
Dementia affects memory, reasoning, and perception. As the brain struggles to make sense of the world, suspicions and delusional thinking may start to occur. Lost items may become “stolen”, forgotten conversations never happened, unfamiliar faces (even loved ones) feel threatening, and/or gaps in memory may be filled in with made-up stories or beliefs.
Suspicion often shows up as unfounded beliefs that someone is doing something wrong — like hiding belongings or talking behind their back. Delusions are false beliefs that aren't based in reality — such as believing a spouse is an imposter, that someone is stealing, or that people are in the house when no one is there. These behaviors are symptoms of the disease — not a reflection of your relationship or the care you are providing.
Tips for Caregivers
- Don’t Take It Personally
Remember that this is the disease talking, not your loved one. Accusations can be hurtful, but they aren’t intentional. - Stay Calm and Reassuring
Arguing or trying to convince them they’re wrong usually only creates more suspicion. Instead, offer gentle reassurance: “I understand how that is upsetting to you. Let’s look for your wallet together.” - Redirect and Distract
If possible, shift the focus to a different activity — a snack, music, or a favorite photo album. - Create a Sense of Security
Keep familiar items visible, label drawers or cabinets, and maintain a predictable routine to reduce anxiety and confusion. - Use Validation, Not Correction
Instead of “No one’s stealing from you,” try validating their feelings. Saying something like “You’re feeling worried about your things. Let’s make sure everything is in the right place” may be more effective.
Final Thoughts
Suspicion and delusions are difficult parts of dementia — both for the person with dementia and for the people caring for them. It is important to remember that they are symptoms, not personal attacks or a reflection on the care being provided. Responding with calm, compassion, and flexibility can ease the tension and protect your relationship.
Understanding Wandering
Wandering is one of the most concerning behaviors caregivers deal with when supporting someone with dementia. A person may leave the house unexpectedly, pace for long periods, or try to "go home” —even if they’re already there. While wandering can be frightening, it’s also common, especially in the middle and later stages of dementia.
Wandering is often caused by a need the person can’t express clearly. Some of the most common reasons for wandering are confusion about where they are and what time it is, following past routines (like going for a walk or commuting to work), restlessness or boredom, looking for something or someone familiar, and/or feeling anxious or fearful.
Caregiver Tips
- Be Aware of Signs Someone May Be at Risk of Wandering
Even before someone wanders, there may be signs such as trying to “go home” when already there, talking about needing to go to work, pacing or fidgeting, attempting to open doors to leave. - Create a Safe, Structured Environment
Maintain a daily routine to reduce confusion and restlessness. Keep the environment calm, familiar, and engaging. - Secure Exits Thoughtfully
Consider using childproof doorknob covers, door alarms, or motion sensors. Placing a dark mat in front of the door or painting it the same color as the wall may discourage exit attempts. - Keep Keys and Shoes Out of Sight
These can be visual cues that trigger the urge to leave. - Provide Safe Ways to Move
Regular walks or gentle physical activity can satisfy the need to move, helping prevent restlessness. - Use Identification Tools
Make sure your loved one wears an ID bracelet or medical alert tag. You might also consider GPS tracking devices designed for dementia care. - Alert Neighbors and Local Support
Let trusted neighbors or nearby friends know about the situation in case your loved one leaves home unexpectedly.
Final Thoughts
Wandering is a symptom of dementia, often caused by a need the person can’t clearly express. By understanding the triggers for wandering and taking steps to prevent it, you can help keep your loved one safe while giving yourself greater peace of mind.
Providers
Disease Specific Guidelines for Hospice Eligibility
Amyotrophic Lateral Sclerosis (ALS)
The patient meets at least one of the following:
- Severely impaired breathing capacity with all the following findings:
- Dyspnea at rest
- Vital capacity less than 30%
- Requirement for supplemental oxygen at rest
- The patient declines artificial ventilation
OR
- Rapid disease progression as evidenced by all the following in the preceding 12 months (with either a or b below):
- Progression from independent ambulation to wheelchair or bed-bound status
- Progression from normal to barely intelligible or unintelligible speech
- Progression from normal to pureed diet
- Progression from independence in most or all Activities of Daily Living (ADL) to needing major assistance by caretaker in all ADL
A. Severe nutritional impairment demonstrated by all the following in the preceding 12 months:
- Oral intake of nutrients and fluids insufficient to sustain life
- Continuing weight loss
- Dehydration or hypovolemia
- Absence of artificial feeding methods
B. Life-threatening complications demonstrated by one or more of the following in the preceding 12 months:
- Recurrent aspiration pneumonia (with or without tube feeding)
- Upper urinary tract infection (Pyelonephritis)
- Sepsis
- Recurrent fever after antibiotic therapy
- Stage 3 or Stage 4 pressure ulcer(s)
Rapid decline or comorbidities may support eligibility for hospice in the absence of one or more of these findings.
Alzheimer's Disease and Related Disorders
The patient has both 1 and 2:
- Stage 7 or beyond according to the Functional Assessment Staging Scale (FAST) with all the following:
- Inability to ambulate without assistance
- Inability to dress without assistance
- Inability to bathe without assistance
- Urinary and fecal incontinence, intermittent or constant
- No consistent meaningful/reality-based verbal communication, or the ability to speak is limited to a few intelligible words
AND
- Has had at least one of the following conditions within the past 12 months:
- Aspiration pneumonia
- Pyelonephritis or other upper urinary tract infection
- Septicemia
- Pressure ulcers, multiple and/or Stage 3 or Stage 4
- Fever, recurrent after antibiotics
- Inability to maintain sufficient fluid and caloric intake demonstrated by either of the following: 10% weight loss during the previous six months OR Serum albumin <2.5gm/dl
Rapid decline or comorbidities may support eligibility for hospice in the absence of one or more of these findings.
Cancer
The patient has 1, 2 and 3:
- Clinical findings of malignancy with widespread, aggressive or progressive disease as evidenced by increasing symptoms, worsening lab values and/or evidence of metastatic disease
AND
- Impaired performance status with a Palliative Performance Score (PPS) <70%
AND
- Refuses further curative therapy or continues to decline despite definitive therapy. Decline is evidenced by:
- Hypercalcemia greater than or equal to 12
- Cachexia or weight loss of 5% in the preceding three months
- Recurrent disease after surgery/radiation/chemotherapy
- Signs and symptoms of advanced disease, e.g., nausea, anemia, malignant ascites or pleural effusion, etc.
The following information will be required: Tissue diagnosis of malignancy OR reason(s) why a tissue diagnosis is not available Certain cancers with poor prognoses (e.g. small cell lung cancer, brain cancer and pancreatic cancer) may be hospice eligible without fulfilling the other criteria in this section. Rapid decline or comorbidities may support eligibility for hospice in the absence of one or more of these findings.
Heart Disease
The patient has 1 or 2, and 3:
- Poor response to (or patient’s choice is not to pursue) optimal treatment with diuretics, vasodilators and/or angiotensin converting enzyme (ACE) inhibitors
OR
- The patient has angina pectoris at rest resistant to standard nitrate therapy and is not a candidate for invasive procedures and/or has declined revascularization procedures
AND
- New York Heart Association (NYHA) Class IV symptoms with both of the following:
- The presence of significant symptoms of recurrent Congestive Heart Failure (CHF) and/or angina at rest
- Inability to carry out even minimal physical activity with symptoms of heart failure (dyspnea and/or angina)
Supporting evidence for hospice eligibility:
- Echo demonstrating an ejection fraction of 20% or less
- Treatment-resistant symptomatic dysrhythmias
- History of unexplained or cardiac related syncope
- CVA secondary to cardiac embolism
- History of cardiac arrest or resuscitation
- Brain embolism of cardiac origin
- Concomitant HIV disease
Rapid decline or comorbidities may support eligibility for hospice in the absence of one or more of these findings.
HIV Disease
The patient is considered in the terminal stage of their illness (life expectancy of six months or less) if they meet the following conditions.
- CD4+ count <25 cells/mm3
OR
- Persistent viral load >100,000 copies/ml
AND
- At least one of the following conditions:
- CNS lymphoma
- Untreated or not responsive to treatment; wasting (loss of 33% lean body mass)
- Mycobacterium avium complex (MAC) bacteremia, untreated, unresponsive to treatment or treatment refused
- Progressive multifocal leukoencephalopathy
- Systemic lymphoma with advanced HIV disease and partial response to chemotherapy
- Visceral Kaposi's sarcoma unresponsive to therapy
- Renal failure in the absence of dialysis
- Cryptosporidium infection
- Toxoplasmosis unresponsive to therapy
- Cytomegalovirus (CMV) infection
AND
- Palliative Performance Score of <50% (requires considerable assistance and frequent medical care, activity limited mostly to bed or chair)
Documentation of the following factors will support eligibility for hospice care:
- Chronic persistent diarrhea for one year
- Persistent serum albumin <2.5
- Concomitant, active substance abuse
- Age >50 years
- Advanced AIDS dementia complex
Rapid decline or comorbidities may support eligibility for hospice in the absence of one or more of these findings.
Huntington's Disease
The patient has both 1 and 2:
- Stage 7 or beyond according to the Functional Assessment staging scale with all the following
- Inability to ambulate without assistance
- Inability to dress without assistance
- Urinary and fecal incontinence, intermittent or constant
- No consistent meaningful verbal communication
AND
- Has had at least one of the following conditions within the past 12 months:
- Aspiration pneumonia
- Pyelonephritis or other upper urinary tract infection
- Septicemia
- Multiple Stage 3 or Stage 4 pressure ulcers
- Toxoplasmosis unresponsive to therapy
- Fever, recurrent after antibiotics
- Inability to maintain sufficient fluid and caloric intake with one or more of the following during the preceding 12 months: 10% weight loss during the previous six months OR Serum albumin <2.5 gm/dl OR Significant dysphagia with associated aspiration measured objectively, e.g., swallowing test or a history of choking or gagging with feeding.
In the absence of one or more of these findings, rapid decline or comorbidities may also support eligibility for hospice care.
Liver Disease
The patient has both 1 and 2:
- Synthetic liver failure as demonstrated by: Prothrombin time (PTT) prolonged more than five seconds over control OR International Normalized Ratio (INR) >1.5 AND Serum albumin <2.5 gm/dl.
- End-stage liver disease is present, and the patient has one or more of the following conditions:
- Ascites, refractory to treatment, or patient declines or is non-compliant
- History of spontaneous bacterial peritonitis
- Hepatorenal syndrome (elevated creatinine with oliguria of <400 ml/day)
- Hepatic encephalopathy, refractory to treatment or patient non-compliant
- History of recurrent variceal bleeding despite intensive therapy or patient declines therapy
Supporting evidence for hospice eligibility:
- Progressive malnutrition
- Muscle wasting with reduced strength
- Ongoing alcoholism (>80 gm ethanol/day)
- Hepatocellular carcinoma
- Hepatitis B surface antigen positive
- Hepatitis C refractory to interferon treatment
Patients awaiting liver transplant who otherwise fit the above criteria may be certified for the Medicare hospice benefit, but if a donor organ is procured, the patient should be discharged from hospice. Rapid decline or comorbidities may support eligibility for hospice in the absence of one or more of these findings.
Multiple Sclerosis
The patient must meet the following criteria:
- Severely impaired breathing capacity with all the following findings:
- Dyspnea at rest
- Vital capacity less than 30%
- The requirement of supplemental oxygen at rest
- The patient declines artificial ventilation
OR
- Rapid disease progression as evidenced by all the following in the preceding 12 months:
- Progression from independent ambulation to wheelchair or bed-bound status
- Progression from normal to barely intelligible or unintelligible speech
- Progression from normal to pureed diet
- Progression from independence in most or all Activities of Daily Living (ADLs) to needing major assistance by caregiver in all ADLs
AND
- Severe nutritional impairment demonstrated by all the following in the preceding 12 months:
- Oral intake of nutrients and fluids insufficient to sustain life
- Continuing weight loss
- Dehydration or hypovolemia
- Absence of artificial feeding
OR
- Life-threatening complications demonstrated by one or more of the following in the preceding 12 months:
- Recurrent aspiration pneumonia (with or without tube feedings)
- Upper urinary tract infections (e.g. Pyelonephritis)
- Sepsis
- Recurrent fever after antibiotic therapy
- Stage 3 or Stage 4 pressure ulcer
In the absence of one or more of these findings, rapid decline or comorbidities may also support eligibility for hospice care.
Muscular Dystrophy
The patient must meet at least one of the following criteria:
- Severely impaired breathing capacity with all the following findings:
- Dyspnea at rest
- Vital capacity less than 30%
- The requirement of supplemental oxygen at rest
- The patient declines artificial ventilation
OR
- Rapid disease progression as evidenced by all the following in the preceding 12 months:
- Progression from independent ambulation to wheelchair or bedbound status
- Progression from normal to barely intelligible or unintelligible speech
- Progression from normal to pureed diet
- Progression from independence in most or all Activities of Daily Living (ADLs) to needing major assistance by caregiver in all ADLs
AND
- Severe nutritional impairment demonstrated by all the following in the preceding 12 months:
- Oral intake of nutrients and fluids insufficient to sustain life
- Continuing weight loss
- Dehydration or hypovolemia
- Absence of artificial feeding
OR
- Life-threatening complications demonstrated by one or more of the following in the preceding 12 months:
- Recurrent aspiration pneumonia (with or without tube feedings)
- Upper urinary tract infections (e.g. Pyelonephritis)
- Sepsis
- Recurrent fever after antibiotic therapy
- Stage 3 or 4 pressure ulcer(s)
In the absence of one or more of these findings, rapid decline or comorbidities may also support eligibility for hospice care.
Parkinson's Disease
The patient must meet the following criteria from 1, and 2 or 3:
- Rapid disease progression
- Progression from independent ambulation to wheelchair or bedbound status
- Progression from normal to barely intelligible or unintelligible speech
- Progression from normal to pureed diet
- Progression from independence in most or all Activities of Daily Living (ADLs) to needing major assistance by caregiver in all ADLs
AND
- Severe nutritional impairment demonstrated by all the following in the preceding 12 months:
- Oral intake of nutrients and fluids insufficient to sustain life
- Continuing weight loss
- Dehydration or hypovolemia
- Absence of artificial feeding
OR
- Life-threatening complications demonstrated by one or more of the following in the preceding 12 months:
- Recurrent aspiration pneumonia (with or without tube feedings)
- Upper urinary tract infection (e.g. Pyelonephritis)
- Sepsis
- Recurrent fever after antibiotic therapy
- Stage 3 or Stage 4 pressure ulcer(s)
Rapid decline or comorbidities may support eligibility for hospice in the absence of one or more of these findings.
Pulmonary Disease
The patient has severe chronic lung disease as documented by the following:
- Disabling dyspnea at rest, AND
- Poor response to bronchodilators, AND
- Decreased functional capacity, e.g., bed to chair existence, fatigue and cough (An FEV1 <30% is objective evidence for disabling dyspnea but is not required)
AND
- Progression of disease as evidenced by a recent history of increased visits to MD office, home or emergency room and/or hospitalizations for pulmonary infections and/or respiratory failure
AND
- Documentation within the past three months of: Hypoxemia at rest (pO2<55 mgHg by ABG) or oxygen saturation <88% OR Hypercapnia evidenced by pCO2>50 mm Hg
Supporting evidence for hospice eligibility:
- Cor pulmonale and right heart failure secondary to pulmonary disease
- Unintentional progressive weight loss >10% over the preceding six months
- Resting tachycardia >100 bpm
Rapid decline or comorbidities may support eligibility for hospice in the absence of one or more of these findings.
Renal Disease
The patient has 1 and either 2 or 3:
- The patient is not seeking dialysis or transplant (there may be circumstances when dialysis is used as a concurrent therapy or is not related to the patient’s primary hospice diagnosis and the patient may be eligible for hospice)
AND
- Creatinine clearance <10cc/min (<15cc/min for diabetics)
OR
- Serum creatinine >8.0 mg/dl (>6.0 mg/dl for diabetics)
Comorbid conditions that lend supporting documentation:
- Mechanical ventilation
- Malignancy (other organ system)
- Chronic lung disease
- Advanced cardiac disease
- Advanced liver disease
- Sepsis
- Immunosuppression/AIDS
- Albumin
- Cachexia
- Platelet count <25,000
- Disseminated intravascular coagulation
- Gastrointestinal bleeding
Supporting evidence for hospice eligibility:
- Uremia
- Oliguria (urine output is less than 400 cc in 24 hours)
- Intractable hyperkalemia (> 7.0) not responsive to treatment
- Uremic pericarditis
- Hepatorenal syndrome
- Immunosuppression/AIDS
- Intractable fluid overload, not responsive to treatment
Rapid decline or comorbidities may support eligibility for hospice in the absence of one or more of these findings.
Stroke or Coma
The patient has both 1 and 2:
- Poor functional status with Palliative Performance Score of 40% or less (unable to care for self)
AND
- Poor nutritional status with inability to maintain sufficient fluid and calorie intake with either:
- >10% weight loss over the previous six months
- >7.5% weight loss over the previous three months
- Serum albumin <2.5 gm/dl
- Current history of pulmonary aspiration without effective response to speech language pathology interventions to improve dysphagia and decrease aspiration events
Supporting evidence for hospice eligibility: Coma (any cause) with three of the following on the third day of coma:
- Abnormal brain stem response
- Absent verbal responses
- Absent withdrawal response to pain
- Serum creatinine >1.5 gm/dl
For non-traumatic hemorrhagic stroke:
- Large-volume hemorrhage on CT:
- Infratentorial: ≥20 ml
- Supratentorial: ≥50 ml
- Ventricular extension of hemorrhage
- Surface area of involvement of hemorrhage ≥30% of cerebrum
- Midline shift ≥5 cm
- Obstructive hydrocephalus in patient who declines, or is not a candidate for, ventriculoperitoneal shunt
For thrombotic/embolic stroke:
- Large anterior infarcts with both cortical and subcortical involvement
- Large bi-hemispheric infarcts
- Basilar artery occlusion
- Bilateral vertebral artery occlusion
In the absence of one or more of these findings, rapid decline or comorbidities may also support eligibility for hospice care.
Alternative Pain Scales
The FLACC Scale is a behavioral pain assessment scale used for nonverbal patients who are unable to self-report their level of pain. To assess pain level, rate the patient in each of the five categories and add results together to determine total pain score. 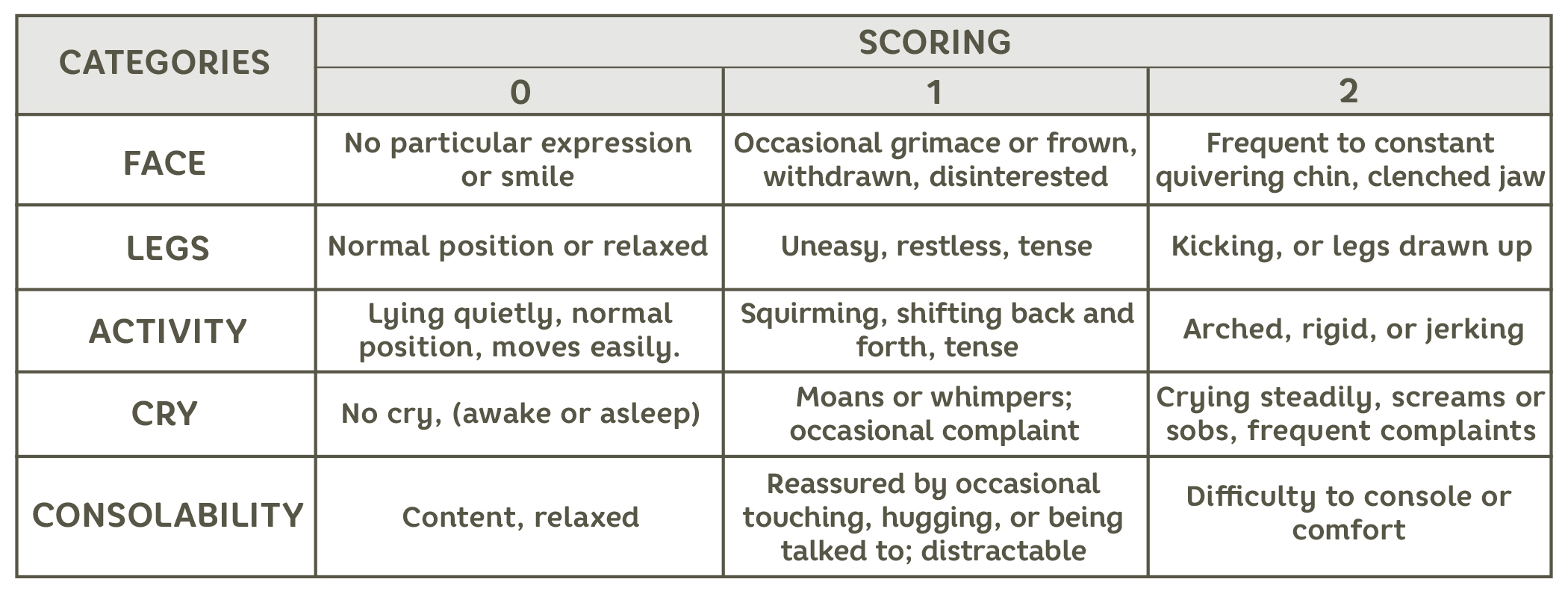
Staging Tool for Dementia
The FAST Scale was developed to measure the progression of pure Alzheimer’s disease. An individual’s FAST score relates directly to the stage of cognitive decline the person is currently at. Individuals who have Alzheimer’s dementia typically advance through the FAST stages in order. When this scale is used on individuals who have mixed dementia, they may not follow the stages in order, and some may be skipped over entirely.
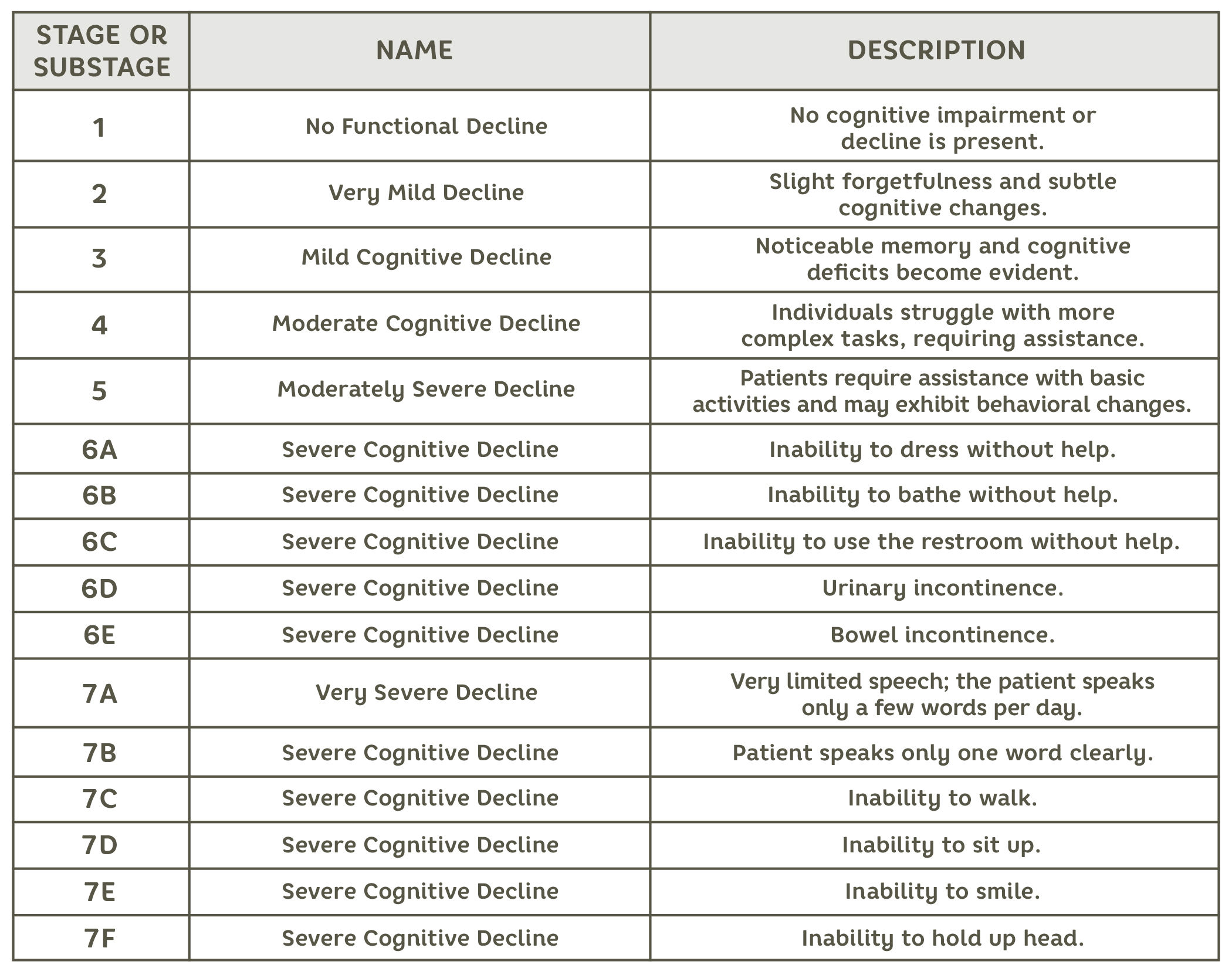
Functional Decline Assessment Tool
Palliative Performance Scale (PPS)
The Palliative Performance Scale is used by healthcare professionals to assess a patient’s functional decline. The PPS Scale can facilitate decisions regarding a patient's hospice or palliative care eligibility. The PPS Scale measures 5 functional domains: ambulation, activity level and evidence of disease, self-care, oral intake, and level of consciousness. 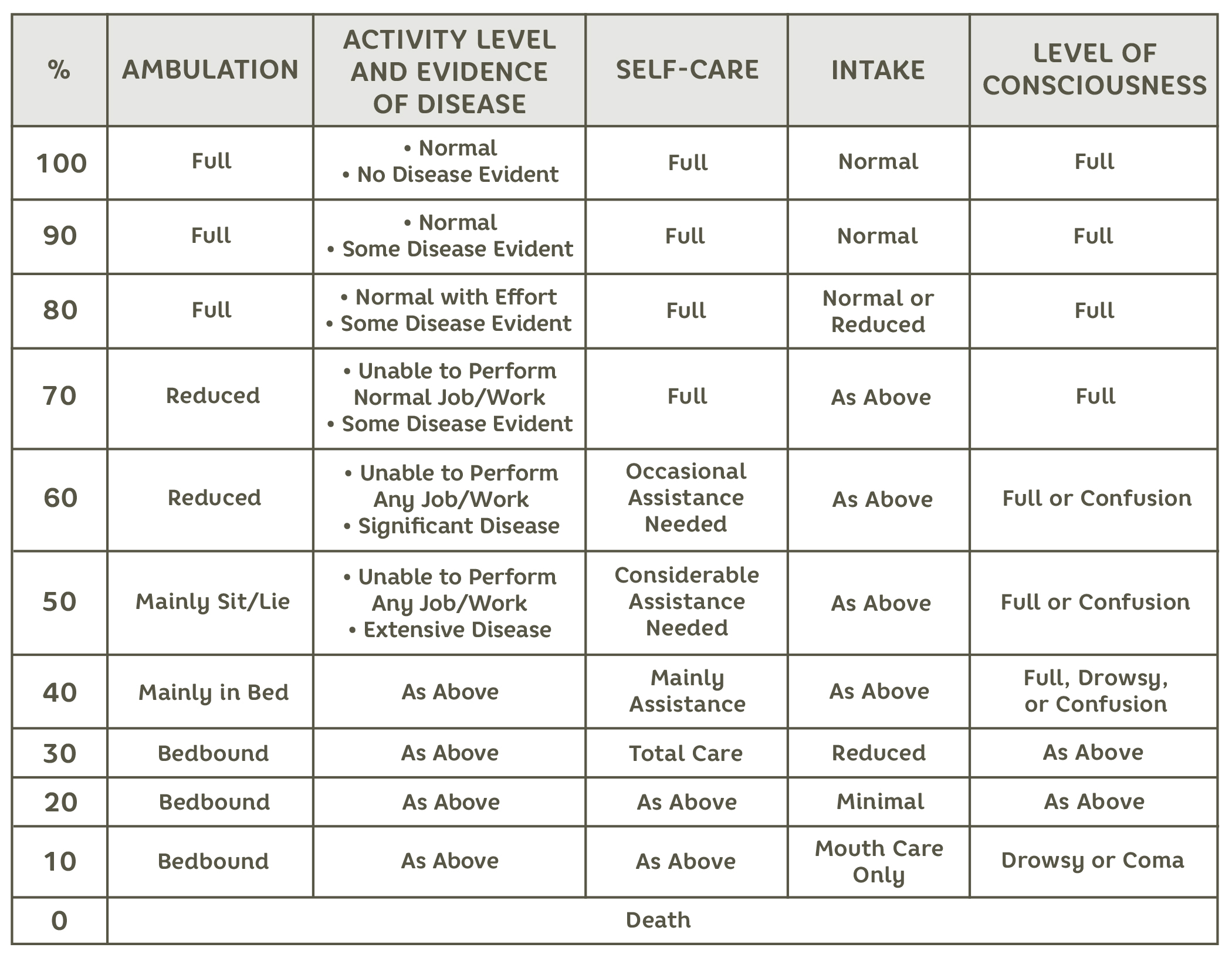
New York Heart Association (NYHA) Functional Classification
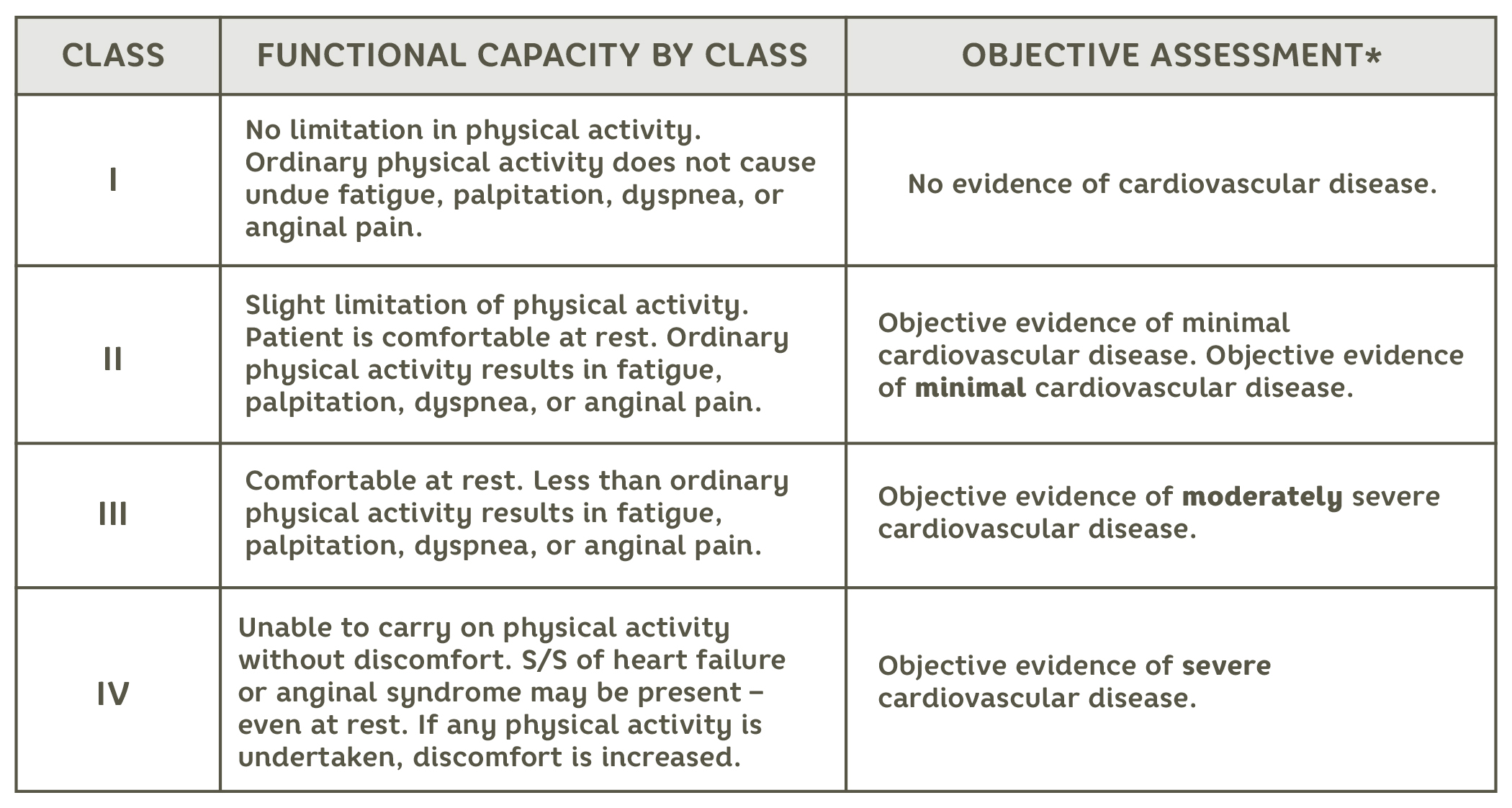
*Measures such as EKG, stress test, x-ray, echocardiogram, and/or radiologic images.
When and How to Refer to Palliative Care
A palliative care referral should be considered for patients who have a serious or chronic illness, regardless of prognosis, and need support in managing symptoms, improving quality of life, and navigating complex medical decisions. Palliative care focuses on alleviating pain, managing symptoms (e.g. pain, nausea, dyspnea), and addressing emotional, social, and spiritual concerns. Referral is appropriate when:
- Symptom management: The patient experiences symptoms that are difficult to manage or side effects from illness or treatments.
- Complex decision-making: The patient or family needs assistance with care planning, including making informed decisions about treatments and goals of care.
- Improving quality of life: The patient desires help in improving comfort and overall well-being, in addition to or in place of curative treatments.
- Chronic conditions: Palliative care enhances quality of life by alleviating symptom burden for patients who have chronic conditions such as cancer, heart failure, COPD, or advanced neurological diseases.
Palliative care can be provided at any stage of illness and is not limited to end-of-life care, so early referral can enhance care throughout the disease trajectory.
When and How to Refer Your Patient to Hospice
Physicians should consider referring to hospice when a patient's illness is terminal, with a prognosis of six months or less to live, and when curative treatments are no longer effective or desired. Key indicators for hospice referral include:
- Advanced, progressive illness: The patient has a life-limiting condition, such as advanced cancer, heart failure, COPD, or neurological diseases, where further treatment won't significantly improve the quality or length of life.
- Focus on comfort: The patient and family prioritize comfort and quality of life over aggressive treatments.
- Frequent hospitalizations or significant symptom burden: The patient experiences escalating symptoms (pain, shortness of breath, confusion) that are difficult to manage.
Referrals are typically made when curative or aggressive treatments no longer align with the patient’s goals and when they are ready to transition to comfort-focused care. Early referrals to hospice allow for more effective symptom management, greater quality of life, and the support of a multidisciplinary team.
Get Help Now


